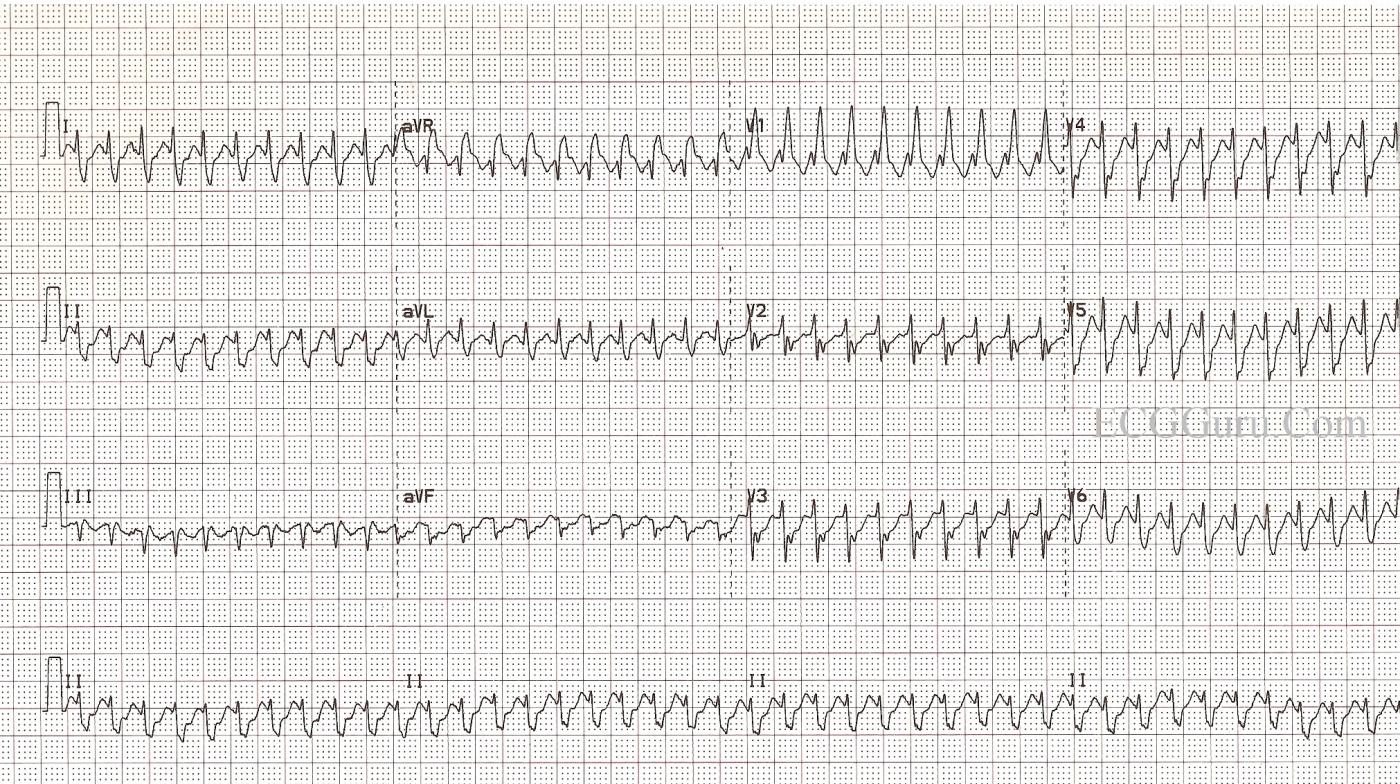
The first ECG is from an active, otherwise healthy 66-year-old man who experienced a sudden onset of symptomatic tachycardia. He presented to the Emergency Dept. feeling (understandably) very anxious, with poor perfusion to his skin, chest discomfort, and palpitations. As the ED staff prepared to electrically cardiovert him, he spontaneously converted to normal sinus rhythm at a rate of 93 / min. and a QRS duration of 90 ms.
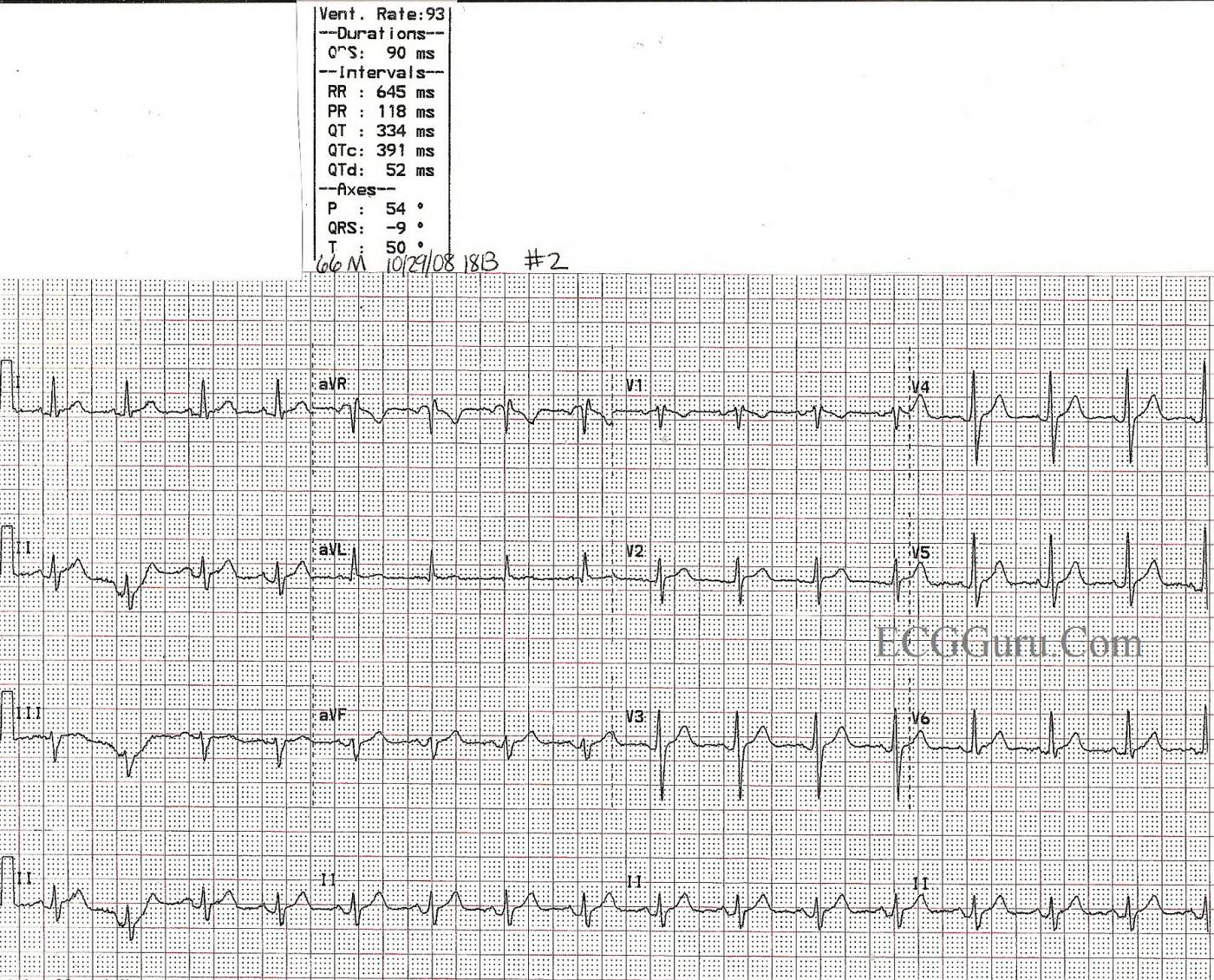
After a normal diagnostic cardiac cath, he was sent to the EP lab and the circuit responsible for this rhythm was successfully ablated. He was discharged in good condition the next day.
This is a good ECG for all levels of students. For beginners, it shows that atrial flutter is one of the rhythms we call "SVT", and it does not always conduct in a variable rate, or a rate that allows "sawtooth" P waves to show easily. You can show them that the "sawtooth" pattern, brought about by P waves that are 250 - 350 per minute, is still there if one ignores the QRS complexes for a moment. This is a great ECG for discussions of rate and cardiac output, and making decisions regarding treatment based on the patient's hemodynamic condition. For more advanced students, this ECG can lead to a discussion of the accessory pathways and re-entrant pathways that cause rapid rhythms. For RBBB criteria, click HERE.
The second ECG shows the same patient after spontaneous conversion to sinus rhythm. The bundle branch block has disappeared, as it was rate-dependent.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Patient Above After Spontaneous Conversion to NSR
This patient presented with atrial flutter 1:1, and a rate-dependent right BBB. He spontaneously converted to NSR.
For a print-quality image, click HERE.
.
Dawn Altman, Admin
Suspecting WPW - Flutter at 300 - Very Fast AFib
GREAT post by Dawn of an uncommon occurrence (flutter at 300/minute) - but one that will on occasion be seen, so good to be aware of. I know of nothing other than atrial flutter that produces a regular rhythm at 300/minute. Untreated AFlutter most often conducts at 2:1 (atria = 300/min; ventricles = 150/min). The next 2 most common conduction ratios are 4:1 and AFlutter with a variable ventricular response.
Ken Grauer, MD www.kg-ekgpress.com [email protected]