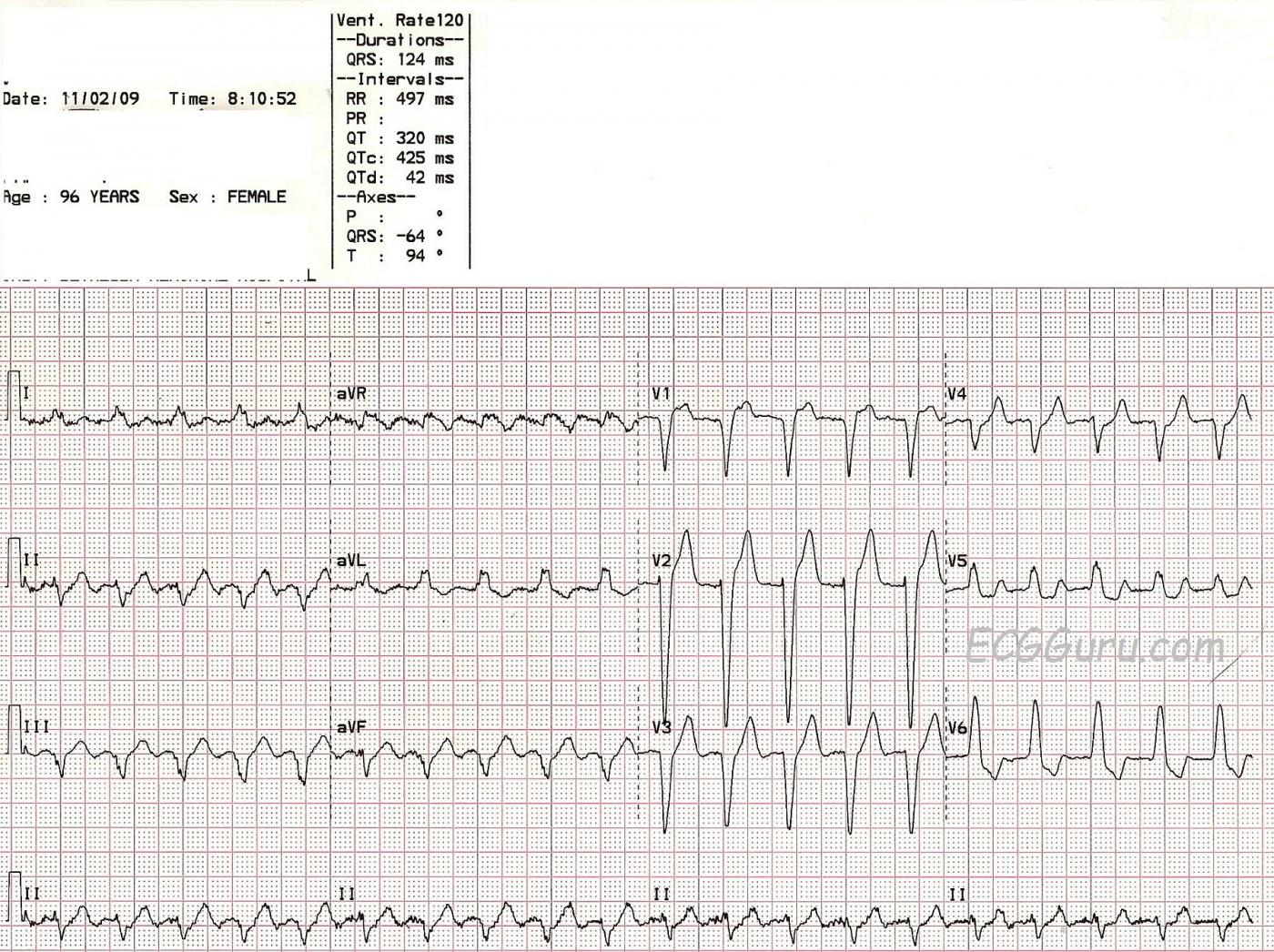
This ECG is a two-for-one teaching opportunity. This elderly woman presents with a tachycardia at about 120/min. We do not have any other information about her complaints or past medical history.
Her ECG shows a wide-complex tachycardia. The QRS complexes are about 124 ms (.12 sec.) wide. On the most basic level, we should teach our students to consider ALL wide-complex tachycardias to be ventricular tachycardia until proven otherwise. This ECG has many clues that it is NOT ventricular tachycardia. Tiny P waves can be seen in V1, V2, and V3. But, these are not the only P waves. The atrial rate in this case is twice the ventricular rate, making the rhythm ATRIAL FLUTTER with 2:1 conduction. The flutter rate is about 240/minute, slightly on the slow side for AFL. Atrial flutter with 2:1 conduction is often missed, as every other P wave is hidden. Look at aVR and Lead II in this case for signs of the regular flutter waves. It is important to look in all 12 leads for signs of flutter waves in any tachycardia over 120/min. Occasionally, you will get lucky, and the patient will conduct at a different ratio, such as 3:1 or 4:1, making the flutter waves much more visable. Sometimes, the atrial flutter becomes apparent during carotid sinus massage or a Valsalva maneuver.
The QRS width, in this case, is due to left bundle branch block. The criteria for LBBB are: Wide QRS, Supraventricular Rhythm (in this case, atrial flutter), and a negative QRS in V1 with a positive QRS deflection in Leads I and V6. The ST changes seen here are typical of LBBB: ST depression in leads with upright QRS complexes and ST elevation in leads with downward QRS complexes.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Which Lead Helps Most in Diagnosing the Rhythm?
Ken Grauer, MD www.kg-ekgpress.com [email protected]