Narrow-complex tachycardias can be very confusing to students of basic-level ECG. There are very many rhythms that fall into the broad category of narrow-complex tachycardia. We usually further divide them into sinus tachycardia and other "supraventricular tachycardias". The basic student will want to make this distinction, as well as be able to differentiate atrial fib and atrial flutter from the other SVTs. The more advanced student will want to go into more detail about which mechanism for supraventricular tachycardia is present.
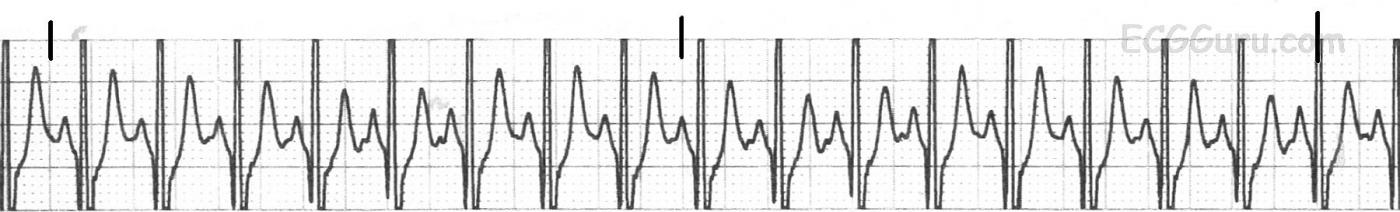
Just the basics, please. When the tachycardia is regular, it is most important to determine whether it is a SINUS TACHYCARDIA or a SUPRAVENTRICULAR TACHYCARDIA. (Yes, we are aware that sinus rhythms are supraventricular, but the term "supraventricular tachycardia" or "SVT" is usually reserved for the fast, regular rhythms that are not sinus.) So, what clues will be most helpful to our beginner students?
Rate SVTs tend to be faster than sinus tachycardia. More importantly, they are fast regardless of the patient's situation. Sinus tachycardia almost always is reacting to the patient's situation. For instance, a 22-year-old woman resting in a chair with a heart rate of 150 is likely to have an SVT. A 22-year-old woman who is running in a 10 k marathon race and has a heart rate of 160 is responding appropriately to an increased need for oxygen and nutrients to her cells. Sinus tachycardia will ususally be 160 or less, and have an obvious reason for being, such as fever, pain, anxiety, exercise, hypovolemia, hypoxia, or drugs. Unfortunately, many beginning students are told that any narrow-complex tachycardia with a rate of 150 or less is sinus, and over 150 is SVT. While they may be right most of the time, or on the written test they are about to take, this rule should not be applied in "real life". Sinus rhythms can go over 150, and SVTs can be slower than 150. So, what other clues should we be teaching beginners?
Consider the clinical situation Look for an obvious cause for sinus tachycardia. If none is found, strongly consider SVT. Remember that pediatric patients have faster heart rates, especially infants. If the strip is on a test, with no clinical information, consider these:
Onset and offset Since we develop sinus tachycardia as a reaction to some other condition, the onset of the faster rate will be gradual. That is, each beat will be closer to the last until maximum rate is reached. This may take only a few beats, but there will be a gradual lengthening of the R-to-R intervals. SVT, on the other hand, will usually begin very abruptly, with a premature atrial contraction (PAC). From that beat forward, there is a fast, regular rhythm. We call this paroxysmal supraventricular tachycardia, because it begins paroxysmally. These rhythms usually END abruptly, as well. If we are fortunate to see the onset or offset of the tachycardia, we will know whether it is sinus or ectopic in origin.
P waves Sometimes, a tachycardia is so fast that P waves are buried in the preceding T waves and we can't evaluate them. This can make it difficult to differentiate between sinus tachycardia and PSVT. It helps to have multiple leads, especially a 12-lead ECG, because P waves show up better in some leads than in others. Suggest to your students that they check Leads II and V1 if they have the option. PSVT rhythms are often REENTRANT rhythms, caused by a circular conduction pathway that allows one impulse to circle around and reenter the ventricles. These rhythms often have retrograde P waves, which will be negative in the inferior leads (II, III, aVF). SVTs may also have P waves that are after the QRS. Also, the P waves in an ectopic tachycardia will usually look different than the sinus P waves. So, if we catch the onset of the tachycardia, and it is sudden, with a change in the appearance of the P waves, we are certain to have a PSVT.
Response to treatment. Sinus tachycardia may respond temporarily to a Valsalva maneuver, or bearing down, but it will return because the cause of the sinus tachycardia is still present. Supraventricular tachycardia often is stopped by a Valsalva maneuver or carotid sinus massage. Sinus tachycardia usually responds promptly to addressing its cause - relieving pain, reducing fever, calming anxiety, etc.
It helps to give the students factual information, even when it is necessary to simplify. That way, when they go on to more advanced training, they do not have to "unlearn" factoids they have memorized. I have had to help students "unlearn" the 150 per minute "rule" hundreds of times. And, thanks to the widespread use of rhythm generators for training, many people firmly believe that "sinus tach has a P wave and a T wave and SVT has only a T-P".
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
A few more thoughts on sinus tachycardia and SVT...
Dawn...
A great topic and one that is especially pertinent if the person reading the ECG is also responsible for the management of the patient.
I think you were spot on when you made the point that an SVT needs no reason to be present but a patient with a sinus tachycardia will always demonstrate a rather obvious reason for the tachycardia - except for two very rare instances: SA nodal reentry and idiopathic sinus tachycardia. In over 35 years of practice I cannot recall ever having knowingly seen a patient with SA nodal reentry. The only way to recognize it is to actually be recording the ECG when the reentry circuit abruptly begins or abruptly ends. One can certainly suspect it when seeing a patient with sinus P waves at a rate greater than 100 (up to 120 or so) with upright P waves in Leads I and II that precede each QRS complex at a consistent and conductible interval - with no apparent reason for the tachycardia. The patient should also give a history of an abrupt onset of the tachycardia without any provoking stimulus.
I have seen two cases of idiopathic chronic sinus tachycardia. Both were women in their thirties and both had already been diagnosed and advised me of their diagnosis.
But those are very rare conditions.
One thing I would like to point out is that anyone with a supraventricular tachycardia - and especially someone experiencing it for the first time - can be very anxious. Remember: anxiety = adrenalin! Depending on their level of anxiety, some of these patients can produce enough adrenalin to make conversion by vagal means virtually impossible. Adenosine will usually work but even then you may have to give more than one dose. Also, when the patient is converted to sinus rhythm, he/she may be converted to a sinus tachycardia that isn't much less rapid than the SVT they were experiencing. During my years of practice, whenever I was trying to convert a patient (especially before adenosine was available), I would give them some mild sedation first if they appeared very anxious.
Reentrant SVTs will be very, very regular and they don't usually jump from one rate to another and then another. Conversion will be all-or-nothing. If you think the patient has converted but aren't sure, look for upright P waves in front of each QRS complex or deforming the preceding T wave. If you still can't see any, try a vagal maneuver. If the rate slows even momentarily, then the patient is no longer experiencing reentry. Or better yet, use your bedside manner to stand by the patient's bedside for a few minutes, talking to them calmly about things other than their tachycardia while watching the monitor. You will most likely see the heart rate begin to decline very shortly.
Another supraventricular tachycardia that bears mentioning - and one that you will encounter at some point - is atrial tachycardia. Atrial tachycardia is not very common, but it isn't exactly rare, either. It can look just like a sinus tachycardia if it is relatively slow (140 or so). However, atrial tachycardias can also be very rapid (> 200/min). The main problem with atrial tachycardias is that they are not nodal-dependent: vagal maneuvers and adenosine aren't going to help (actually, adenosine will occasionally stop a focal atrial tachycardia but surprisingly has little or no effect on a reentrant atrial tachycardia - go figure!). Generally, medications will not affect it and not even electrical cardioversion will stop it. If 2:1 AV conduction is present, then the tachycardia certainly is not likely to be originating in the sinus node.
Dawn, thanks for a geat blog and the opportunity to post on it.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd