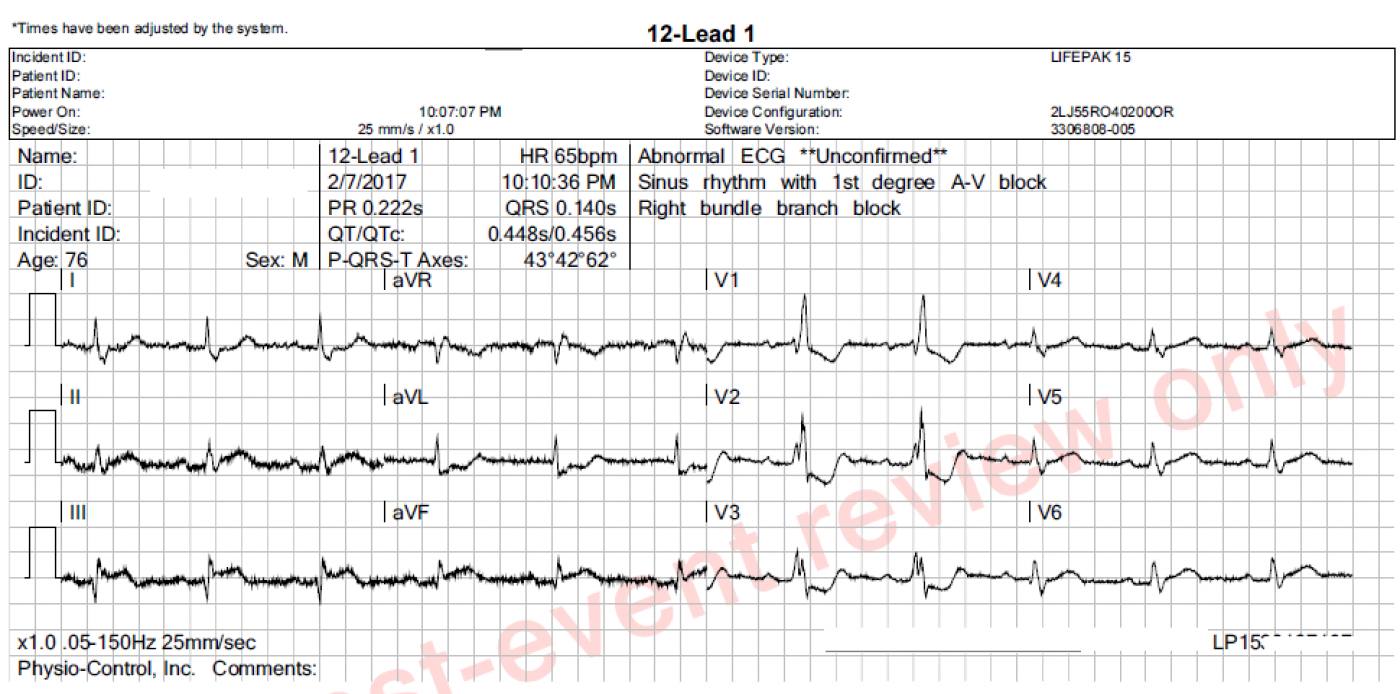
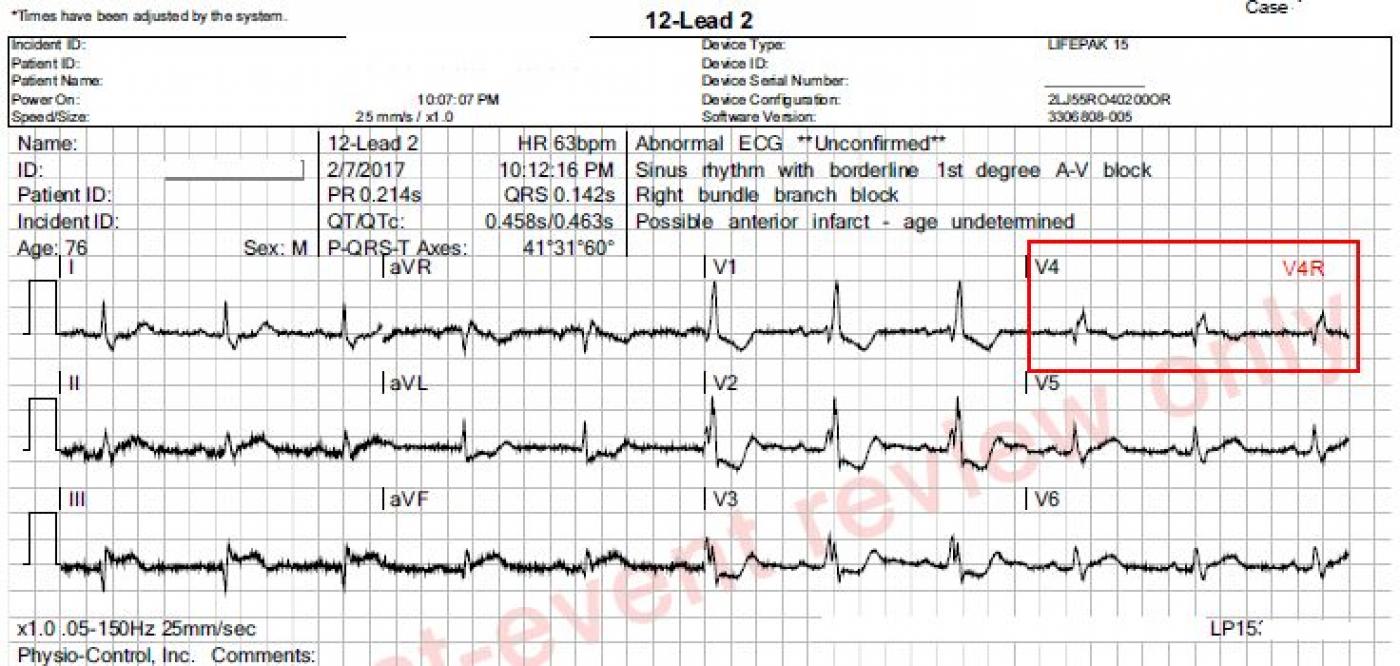
These ECGs were taken from a 76 year-old-man who was complaining of chest pressure for 20 minutes. He had a remote history of coronary artery bypass graft surgery.
This case has several good teaching points, including:
Significant artifact. The limb leads show artifact which is severe enough to hamper our assessment of the j point location. Every effort should be made to eliminate artifact. Some measures that might help are:
* clean and slightly "rough up" the skin where the electrode will be placed. A rough wash cloth or gauze pad will work.
* shave hair if necessary.
* avoid areas of movement if possible. Precordial electrodes must be placed in specific spots, but limb leads may be placed anywhere on the limb or on the trunk if it is impossible to avoid movement on the limbs.
* use fresh electrodes that have been protected from drying out.
Subtle STEMI changes. This patient has an inferior wall M.I., which was confirmed as a complete occlusion of the right coronary artery in the cath lab. The ST elevation in Leads II, III, and aVF is subtle, and more difficult to measure because of the artifact. However, the SHAPE of the ST segments is a giveaway - they are very straight. A convex-upward shape is normal (see Lead I). Also, Lead aVL shows typical ST DEPRESSION, as a reciprocal view of the STE in Lead III. More ST depressions can be seen in Leads V1 through V3, and they end abruptly there. These localized ST depressions represent a reciprocal view of the posterior (also called lateral) wall, and represent an "extension" of the inferior wall M.I. up the back of the heart. A V4 Right lead was obtained and shows no measurable ST elevation, but the shape is straight to slightly "frowning", indicating that the right ventricle may soon have STE. Repeat ECGs should be obtained to watch for more definite ST elevations.
Other findings. The rhythm is sinus at 63 bpm. This is a desirable rate for someone who is having an M.I., as the slower rate protects the heart from damage. Unless the patient is taking rate-slowing medications like beta blockers, the slower rate may be due to the inferior wall M.I. The sinus node has the same blood supply as the inferior wall in most people (RCA), and may slow if ischemic. Also, there may be increased vagal tone. Watch for a too-slow rate that may need intervention - the patient's perfusion status is the key. There is also a RIGHT BUNDLE BRANCH BLOCK. This is not significant to the patient's care, as RBBB does not affect cardiac output and does not cause changes of the ST segment. Unlike left bundle branch block, right bundle branch block is not a "mimic" of STEMI.
Patient outcome. The patient was taken to the cath lab immediately and angioplasty and stenting of the RCA was successful. However, he succumbed to a stroke several days after the procedure.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute Infero-Postero-Lateral MI + RBBB
Excellent case by Dawn. I would add the following comments:
i) As per Dawn — Despite the artifact, one CAN see definitive changes of acute evolving STEMI in the inferior leads. In addition ST segment straightening and elevation — there appear to be q waves in each of the inferior leads! This is admittedly challenging to see given the vertical baseline undulations — but there IS suggestion of a slender negative deflection (that is fairly deep in lead III) at the onset of each QRS complex. Finally, at least in the first complex in lead III — there appears to be beginning T wave inversion. That this finding is real is strongly supported by the fact that in addition to the reciprocal ST depression we see in lead aVL — lead aVL also manifests a biphasic T wave with terminal positivity — which is the precise “mirror-image” of that first ST-T wave in lead III that shows beginning T wave inversion.
ii) I’ll emphasize the clinical utility of the reciprocal relationship between ST-T waves in lead III and lead aVL with evolving inferior infarction. Abnormality in lead aVL is such a consistent finding with evolving inferior infarctions — that the diagnosis should be questioned if the ST-T wave in aVL is completely normal. Appreciation of this reciprocal relationship is invaluable in cases when trying to sort out if upwardly concave ST elevation in the inferior leads is likely to be due to a repolarization variant or evolving inferior infarction.
iii) Lead I does not manifest a normal ST-T wave in this case. Instead, there is straightening of the ST segment in this lead. While admittedly subtle — this finding is undoubtedly real given the ST-T wave findings in the inferior leads and aVL. In general, lead aVL (which electrically lies almost exactly opposite to lead III) tends to show more marked reciprocal changes with inferior infarction than are seen in lead I — but much of the time (as in this case) — lead I still WILL show subtle reciprocal abnormality.
iv) As mentioned by Dawn — complete RBBB is present in this case. A typical ST-T wave response to complete RBBB is seen in lead V1 — in which the ST-T wave is oppositely directed to the terminal tall R’. But the ST-T waves in both leads V2,V3 is distinctly ABNORMAL for simple RBBB. If anything, the depth of ST-T wave depression in response to simple RBBB should lessen as one moves across the chest leads. Instead, ST depression is deeper in V2 than it was in V1. In addition, the shape of the ST-T wave depression has changed in leads V2, V3 from what it was in lead V1 (with addition of a distinct terminal T wave positivity in leads V2 ,V3). This ST-T morphology that is seen here in leads V2, V3 is highly characteristic of associated acute posterior infarction.
v) ST-T waves are not normal in leads V5, V6. Instead, there is ST segment straightening, with a hint of J-point ST elevation. This suggests that this tracing in fact reflects acute evolving infero-postero- and lateral infarction.
vi) Clues that the “culprit artery” is the RCA (rather than the LCx) are the presence of more ST elevation in lead III > II —the marked reciprocal ST depression in lead aVL — and the finding that there is more ST elevation in lead III than in lead V6.
Ken Grauer, MD www.kg-ekgpress.com [email protected]