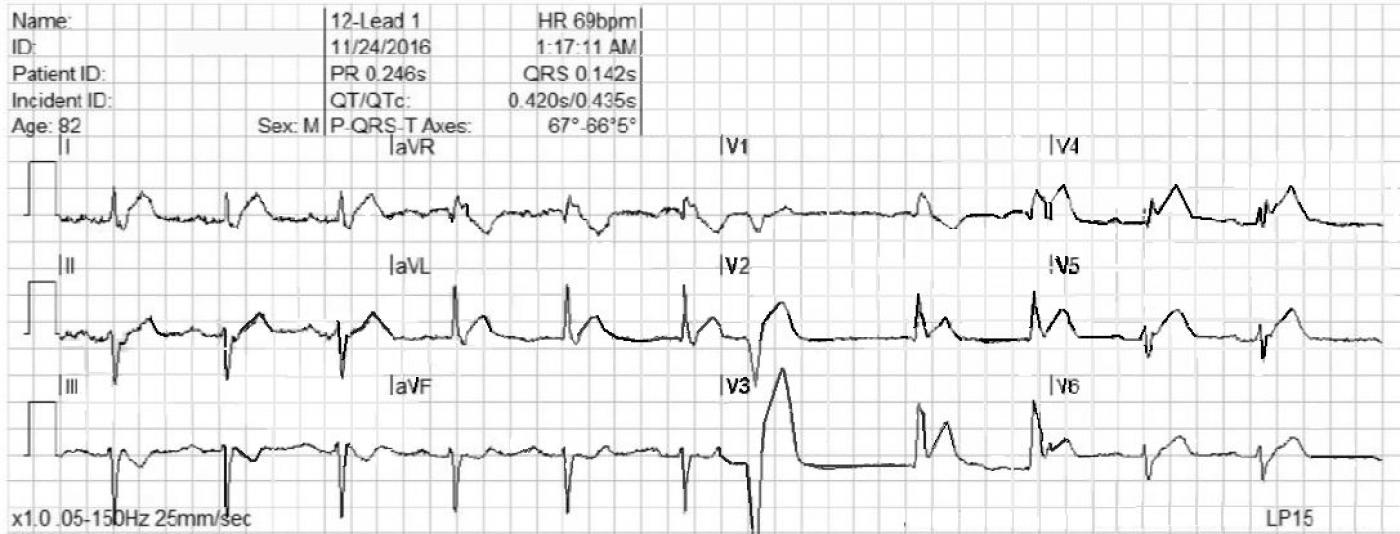
This ECG is taken from an 82-year-old man who called 911 because of chest pain. He has an unspecified “cardiac” history, but we do not know the specifics.
WHAT IS THE RHYTHM? The heart rate is 69 bpm, and there are P waves before every QRS complex. The underlying rhythm is regular, with one premature beat that is wide without a P wave. The PR interval is slightly prolonged at .25 seconds. The rhythm is normal sinus rhythm with first-degree AV block and one PVC.
WHY THE WIDE QRS? The QRS complex is wide at .14 seconds. The QRS in V 1 has a wide R wave after a small Q wave. This in consistent with right bundle branch block pattern, with loss of the normal initial small r wave (pathological Q waves). The diagnosis of RBBB is further corroborated by the wide little S waves in Leads I and V6. The QRS frontal plane axis is -66 degrees per the machine, and clearly “abnormal left” because the QRS in Lead II is negative, while the QRS in Leads I and aVL are positive. This is left anterior fascicular block, also called left anterior hemiblock. The combination of RBBB and LAFB is a common one, as the two branches have the same blood supply. It is also called bi-fascicular block.
WHAT ABOUT THE ST SEGMENTS? The ST segments in leads V2 through V6 are elevated, and their shape is very straight, as opposed to the normal shape of coved upward (smile). Even though the amount of ST elevation at the J points appears subtle, the shape of the segments, the fact that they appear in related leads, and the fact that the patient is an elderly male with chest pain all point to the diagnosis of ANTERIOR WALL ST elevation M.I. (STEMI). Additional ST changes include a straight shape in Leads I and aVL and ST depression in V1 and aVR.
PATIENT OUTCOME The patient was transported to a cardiac center, where he received angioplasty in the cath lab. The left coronary artery was found to be occluded, and was repaired and stented. He recovered without complications and was sent home in a few days.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
How Many Findings of Ant. STEMI Do You See?
Interesting tracing. I’ll add the following comments to Dawn’s interpretation:
1— The rhythm is sinus with 1st-Degree AV Block. In context with other abnormalities on this tracing — this 1st-Degree Block IS significant and may be part of the acute picture.
2— There is 1 PVC. Although it is always more difficult to interpret ST-T wave changes in a PVC — in an 82yo patient with new onset chest pain, the extreme (>10mm) amount of J-point ST elevation in lead V3, with equally disproportionate J-point ST elevation in lead V2 for the PVC is of itself highly suggestive of acute anterior STEMI.
3— As per Dawn, the QRS is wide. QRS morphology is consistent with bifascicular block (RBBB/LAHB) — which has to be assumed acute until proven otherwise. The combination of 1st-Degree AV Block + RBBB/LAHB does NOT by itself definitively localize the conduction defect to the 3rd bundle branch (the cause of prolonged PR interval could be above the His … ) — but it certainly IS possible that there might be trifascicular block …
4— Although it is always more difficult to assess ST-T waves in the setting of RBBB, it clearly is not impossible. There is NO doubt that ST-T waves are HYPERACUTE in leads I, aVL, and V2-thru-V5. In addition, neighboring leads II and V6 are also abnormal (straightening of the ST segment).
5— Confirming the acute MI are the reciprocal ST-T wave changes we see in leads III and aVF. Note in particular the SHAPE of the ST-T wave in lead III. If you flip this ST-T wave from lead III over — you will have a MIRROR-image of the hyperacute ST-T wave that we see in leads I and aVL. This is diagnostic! (along with of course so many other diagnostic features on this tracing).
6— There is a tiny-but-real initial r wave not only in lead V1, but ALSO in leads V2 and V3. This IS significant, and in the context of everything else, signals onset of infarction Q waves.
7— This is a large acute Anterior STEMI in evolution. My guess is that this is a proximal-to-mid LAD occlusion. It’s not Left Main occlusion — because you’d have ST elevation also in V1 with more extreme changes in V1,V2 (and also because if it were a LMain occlusion with these conduction blocks — the patient would most probably have already died). Lack of ST elevation in V1, and relatively less ST elevation in V2 than in V3,V4 suggest that while extensive, it may not be a proximal occlusion.
Ken Grauer, MD www.kg-ekgpress.com [email protected]