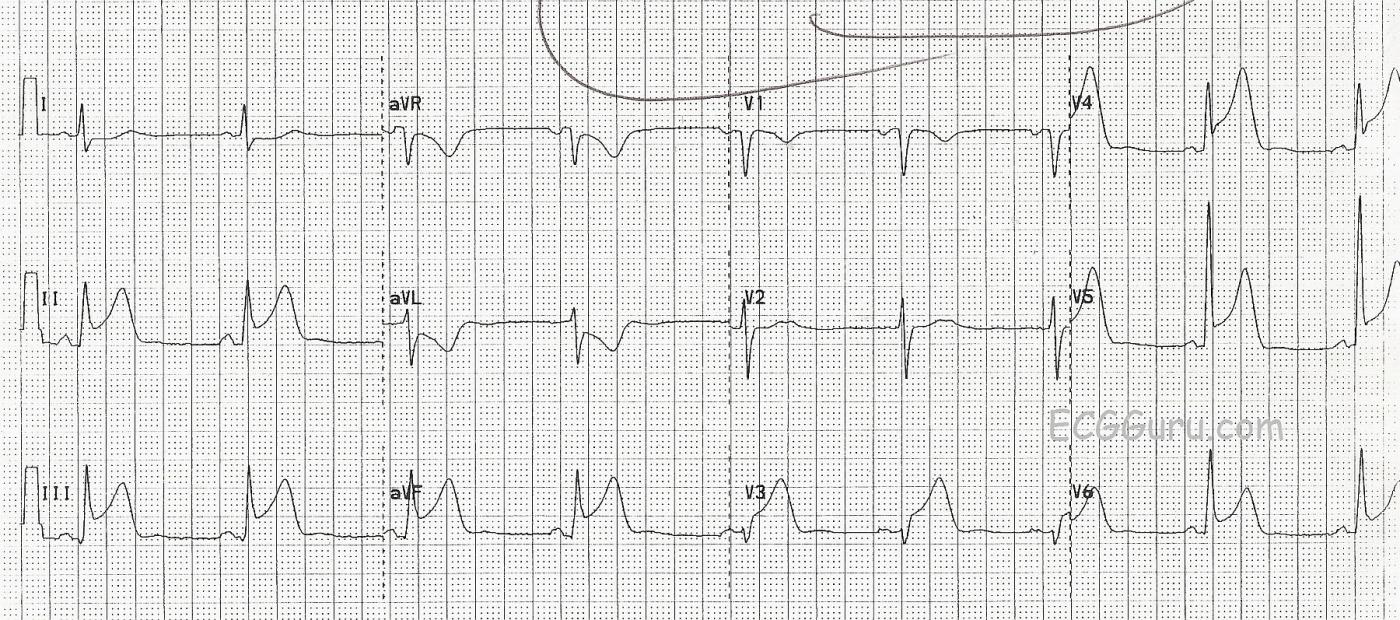
This ECG was obtained from a patient who suffered an obstruction of the circumflex coronary artery. Unfortunately, he was in the approximately 15-18% of the population in whom the circumflex artery is dominant. That means that it connects with the posterior descending artery, perfusing not only the lateral wall of the left ventricle, but also the posterior and inferior walls. In this case, the obstruction is in the midportion of the artery, and the high lateral wall is spared. The large number of leads with ST elevation indicate the large amount of myocardium affected. Leads II, III, and aVF have ST elevation, as do Leads V3 through V6. Lead aVL has reciprocal ST depression. The T waves in the affected leads are "hyperacute", or taller than normal. This is usually an early change in acute M.I., and disappears after the onset of ST elevation.
It is not always easy to determine from the ECG that the circumflex artery is the culprit artery, rather than the right coronary artery, which perfuses the inferior wall in the majority of people. Some clues are: Lead III has ST elevation equal to that of Lead II, the low lateral wall (V5 and V6) are affected, and aVL has reciprocal depression but Lead I does not.
This is a very large M.I., due to the dominance of the circumflex artery. The patient did not survive, in spite of aggressive treatment.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
ST Elevation MI from Which "Culprit" Artery?
Interesting case of this unfortunate patient with obvious acute STEMI who did not survive. Reading between the lines — I surmise that no cardiac catheterization was done — and that the patient died from cardiogenic shock. Without cath documentation, I have reservations on the identity of the “culprit” artery …
Acute inferior STEMI is obvious from marked ST elevation each of the inferior leads. Although it appears that there is slightly more ST elevation in lead III than in lead II (as is expected with acute RCA occlusion) — the difference in ST elevation between these 2 leads is minimal.
The picture in the chest leads however is problematic — as marked ST elevation begins as early as lead V3. The amount of chest lead ST elevation is actually more in leads V3,V4 than it is in V6 — which is not what we’d typically expect with a left dominant circumflex lesion. There IS an R wave in lead V2 — which is then almost lost in V3 — but substantially regained by V4. I wonder about some lead misplacement …
In conclusion — I fully acknowledge not being comfortable in any prediction of coronary anatomy from assessment of this single tracing. I don’t see signs of the usual accompanying posterior involvement (ie, ST depression in anterior leads). Instead — I suspect there may be some lead malposition of V2,V3 — there is marked ST elevation that is maximal in V3,V4 with at-the-least loss of anterior R wave forces, all in association with obvious acute inferior STEMI. My guess would be a mid LAD lesion with inferior “wraparound” — vs multi-vessel disease with some alternative circulation or collateralization — but this is all low-confidence supposition on my part with my intellectual curiosity wondering what an acute catheterization would have shown. Sounds like regardless — the patient succumbed to irreversible cardiogenic shock.
=======================================================
P.S. I have just learned that a cardiac catheterization WAS done on this patient — and it DID show acute occlusion of a dominant left circumflex lesion. Unfortunately, no additional ECGs on this patient can be found — so the question about possible lead misplacement is unanswerable. Just goes to show that one cannot always accurately predict the "culprit artery" from a single ECG ...
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Possible lead misplacement
Thanks, Dr. Ken:
Yes, it is possible there is some lead misplacement. I did not perform this ECG, and, as you know, the concept of correct lead placement is treated lightly by some. I always assumed the exaggerated STs in Leads V3 were due to the proximity of the electrodes to the heart, compared to the distance we see in the left precordial leads. Admittedly, it is unusual to see IWMI due to circumflex occlusion that does not also show some posterior reciprocal changes. I wonder if V1 and V2 were placed too low on the chest?
That being said, I recorded the cath results at the time of the procedure, but did not save the image. One thing I learned in the cath lab is that there is infinite variety in how the coronary arteries are arranged in individuals. It amazed me to see dominant and non-dominant arteries, natural "bypasses", extensive collateralization, and connections between the left and right coronary arteries that caused all to show on angiogram with one injection.
Thanks again for your instructive comments. I hope one take home message from this is that we should all strive for PERFECT electrode placement.
Dawn Altman, Admin
Unusual ECG
Dawn...
It's amazing how the human body refuses to cooperate with all our "rules" and adages regarding ECG interpretation. Like Dr. Grauer, I was thinking more in terms of an RCA lesion based on the ST displacements in Leads II and III. It's ECGs like this that remind us that those "few exceptions to the rule" are always going to be there - especially when certain specialties (like emergency medicine) see a lot of cardiac-related problems and read a lot of ECGs. Perhaps the LCx was dominant enough to irrigate a considerable portion of the RCA area resulting in the Lead III STE > Lead II STE.
The issue of the switched electrode placement (V2 / V3) bothered me. As far as the r wave was concerned, V3 would be more appropriate in V2's place, but then that would give a V1 with no ST deviation, a V2 with marked STE and then a V3 with no ST deviation followed by a V4 with marked STE. The ST changes would be too out of order to make sense.
Perhaps there was a bit of very localized posterior ischemia with V2 reflecting a cancellation of forces. I can't really tell how wide the r wave is in V2, but I would expect it to be at least 0.04 seconds if there was a posterior infarction.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd