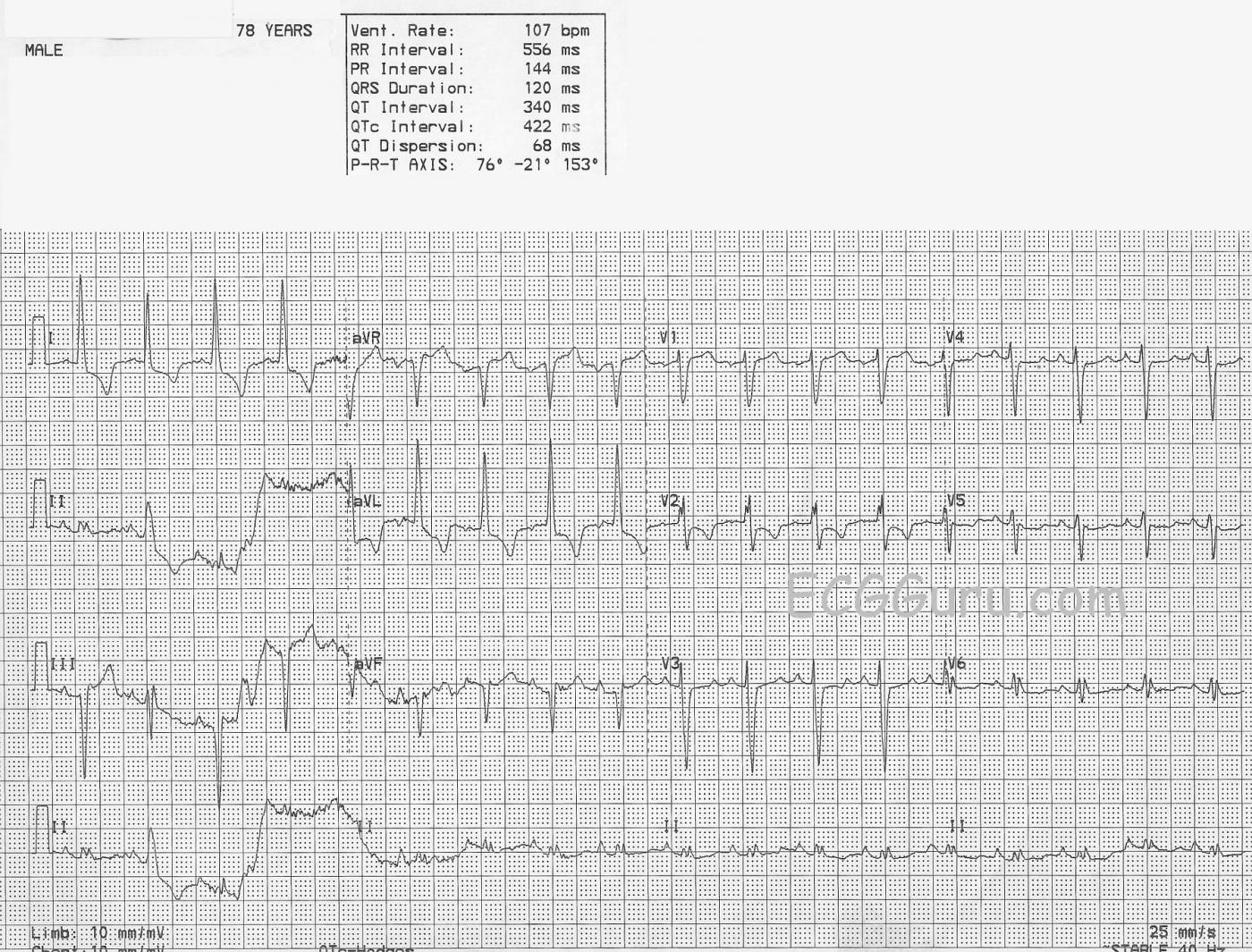
This ECG is being offered as a teaching aid, to show how artifact can affect our ability to interpret an ECG, and to encourage our students to be meticulous in obtaining a good-quality tracing whenever possible. If there are insurmountable obstacles preventing a technically good tracing, the circumstances should be written on the ECG. Such obstacles could be: seizures, tremors, vigorous resuscitation efforts underway, or patient not cooperating.
When an ECG has obvious signs of artifact, the causes of the artifact should be corrected and the ECG repeated. Teach your students to strive for perfection. Even though we cannot obtain “perfection”, if we settle for sloppiness, it will breed more sloppiness.
This ECG has some intriguing abnormal signs, but we should wait for a better tracing before attempting a firm interpretation. We do see abnormal ST segments and T waves in the high lateral leads I and aVL. These, along with the high voltage in aVL, suggest left ventricular hypertrophy with strain. We would expect to see similar signs in the lateral chest leads, V5 and V6, also. The second beat on the ECG appears different from the others, and has a P wave. Even though it is not premature, it could be presumed to have been conducted aberrantly. The precordial leads show poor R wave progression. They should all have an RS pattern, with V1 having a small r wave and a large S wave. The R waves should get more prominent as we move across the chest toward V6, while the s waves become less prominent. So, V1 should be mostly negatively deflected, and V6 should be nearly all positive, with a gradual transition across the chest leads. Poor R wave progression can have many causes. The most preventable one is poor lead placement.
This ECG offers a chance to illustrate to your students why they should understand how each lead is derived. Knowing which limb electrodes are used for each limb lead will lead you, in this case, to the faulty electrode, which may simply be loose. We can see that Lead I is unaffected by the baseline artifact. Lead I is derived from the left and right arm electrodes. Lead II is derived from the left leg and the right arm, and Lead III is derived from the left leg and the left arm. Since Leads II and III are obviously affected by the artifact, which makes the left leg the culprit electrode.
So, rather than encourage your students to try to interpret this ECG, you may want to use it as an example of an ECG with such poor technical quality that it should be repeated.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Assessing Some ECG Technical Aspects
This is a nice example by Dawn that illustrates a number of principles regarding assessment of the technical quality of a tracing. The “bottom line” (as emphasized by Dawn) — is that assuming the clinical situation allows time for it — this ECG should be repeated prior to rendering a definitive interpretation.
The most obvious technical shortcoming is the pronounced artifact + baseline wander in leads II and III. One should therefore look first at the left leg for movement, tremor, faulty lead connection or other technical issues that may be contributing.
Of note — there IS some baseline artifact in lead I (just before the lead switch to lead aVR) — so the left leg isn’t the only problem. And, as one follows the long lead II rhythm strip — much of the artifact is reduced after the initial part of the recording — so some transient problem (ie, tremor, movement, shivering, scratching of the leg, etc.) should be suspected as a likely source of the problem. One look at the patient while the ECG is recorded is often revealing!
There are other technical problems on this tracing. These include improbable progression of QRS morphology for lead V2, which manifests a more prominent (and notched) R wave than we see in lead V3 — as well as a less deep S wave than in either lead V1 or V3. So the usual progression of S wave depth and R wave height is not as expected. The most common cause of this is poor precordial lead placement.
R wave progression and ST-T wave appearance in lateral chest leads is also not what we would anticipate in a patient like this in whom lateral limb leads I and aVL suggest such marked LVH with this extent of ST-T wave abnormalities. So while this precordial lead appearance could be possible — given the technical problems seen in the limb leads, I would hesitate accepting chest lead appearance as valid without first repeating the ECG while verifying lead placement, lead connection, and closely observing the patient for other potential sources of artifact.
BOTTOM LINE: Despite the artifact, I suspect sinus rhythm with marked LVH and ST-T wave changes consistent with ischemia and/or LV “strain”, but without anything acute going on — but, a repeat ECG is needed to know for sure.
Ken Grauer, MD www.kg-ekgpress.com [email protected]