For your collection, we present another interesting set of ECGs from Paramedic Erik Testerman. They are from a 48 year old man who presented responsive only to painful stimuli, with deep, rapid (Kussmaul's) respirations. His blood glucose in the field read as "HIGH" - too high for the glucometer to register a number. He was treated with 3 large-bore IVs, 2 liters of NSS IV, O2. At the hospital, his blood glucose again registered as "HIGH" on the glucometer, arterial O2 was 90%, CO2 15 (low), pH 6.8 (acidotic), HCO3 -2 (depleted). His serum potassium was 7.0 ( greater than 5.5 is high ). We do not have the rest of his chemistry panel.
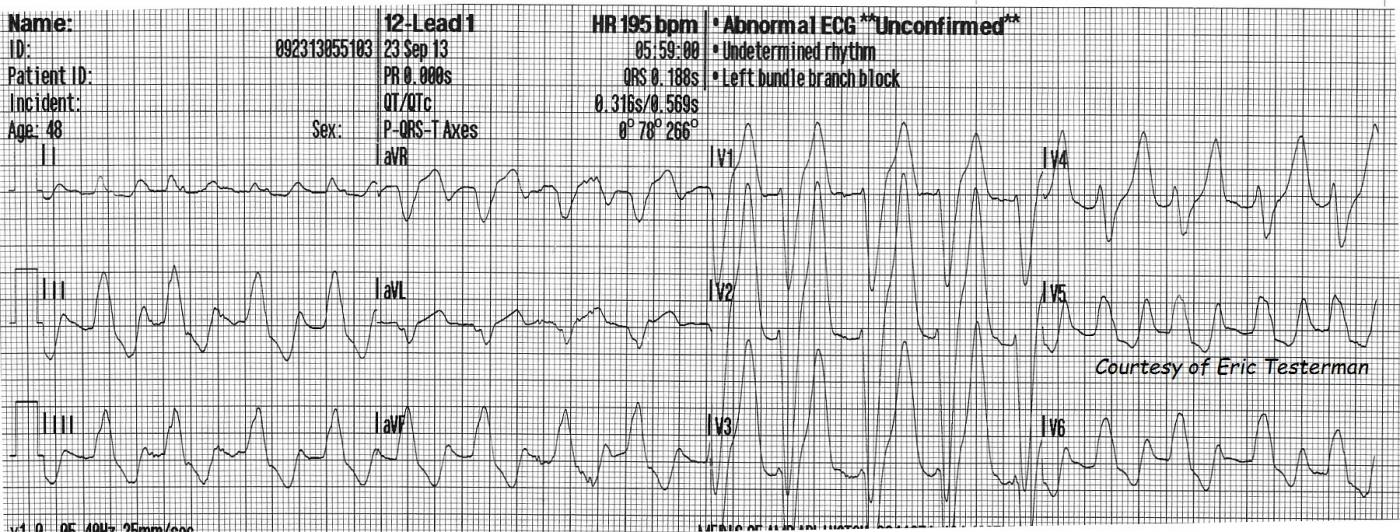
The first ECG, at 5:59 am, shows some signs of early hyperkalemia. One of these signs is wide QRS, at .188 sec (normal is less than .12). This ECG even meets the criteria for LBBB, as noted in the machine's interpretation, but the widening is more likely due to the high potassium. There is a right axis deviation. Left axis deviation is more likely in LBBB. LBBB pattern with right axis deviation can be a sign of biventricular enlargement, but, again, this may be an intraventricular conduction delay that is NOT LBBB. Another sign of hyperkalemia is that P waves are not evident. They can either be flattened until they disappear, or the PR interval can become so long the P wave is lost in the preceding T wave. The T waves are unusually tall and peaked in the chest leads - disproportionate to the wide QRS complexes. There are ST depressions in the inferior leads.
For a good, systematic approach to the ECG changes associated with hyperkalemia, we recommend Life In The Fast Lane, by Ed Burns.
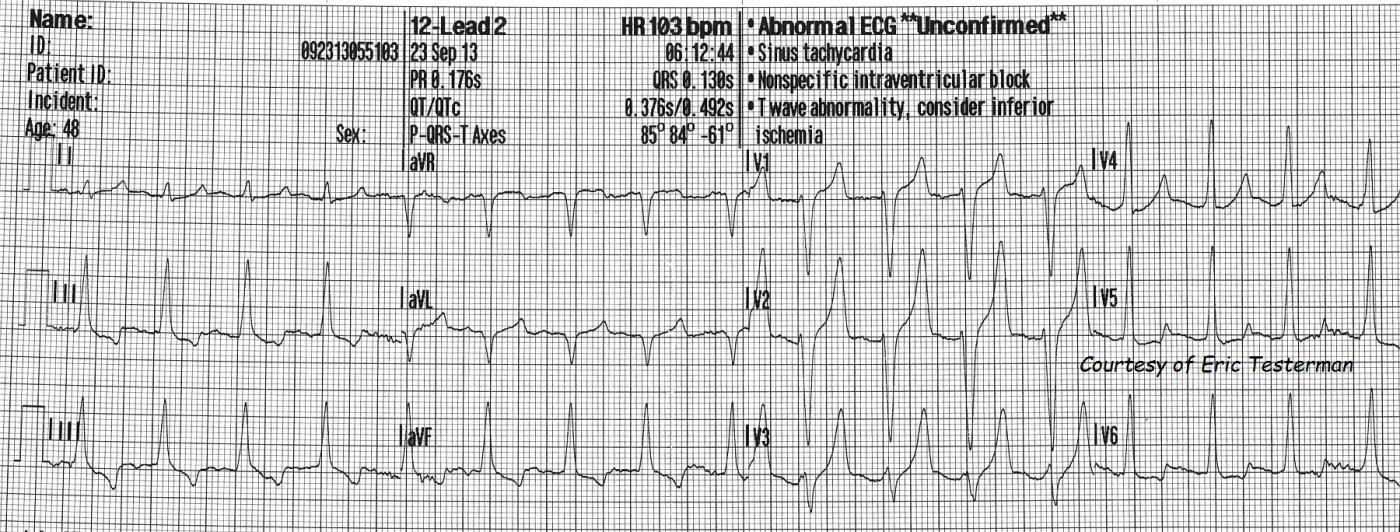
ECG number 2 was taken 13 minutes later, still in the pre-hospital phase. The QRS is now .13 seconds, and the tall, narrow, peaked T waves are very evident in Leads V1 through V3. There is T wave inversion and ST depression in the inferior leads. These are all possible signs of hyperkalemia, but also of other conditions. Unfortunately, hyperkalemia is a "mimic" of many conditions on the ECG. For a very interesting discussion of this topic, please go to Dr. Amal Mattu's ECG Discussion of the Week, October 14, 2013.
Diabetic ketoacidosis and hyperglycemia are frequently associated with hyperkalemia, and it is a potentially deadly consequence of DKA. Unless there are other complicating conditions, the total body potassium is usually not high. The K has been forced out of the cells into the serum. Treatment is aimed at fascilitating K entry into the cells. Once this is accomplished, potassium may need to be replaced. Metabolic acidosis is corrected with Na Bicarb and optimal respiration. Potassium is "pumped" back into the cells by IV calcium followed by insulin and glucose.
The ECG changes of uncorrected hyperkalemia can progress very rapidly from tall, peaked T waves and slightly widened QRS complexes to very wide QRS complexes with no P waves, to sine waves and loss of pulses. It is very important to learn to recognize the ECG signs because they are available immediately, and lab results take time.
Also worth mentioning, especially in cases of hyperkalemia with no ECG changes, pseudo hyperkalelmia has several causes - the most common being traumatic venipuncture. Too much fist-squeezing, tight tourniquets, and rapid, forceful drawing back of the blood from the vein can damage red blood cells, causing release of their intracellular K into the serum in the tube.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
A Tale of 2 Tracings (13 min. apart) with initial QRS Widening
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Littmann's Sign!
As a bit of trivia, the first EKG also exhibits Littmann's sign with a computerized HR double the actual HR. http://www.ncbi.nlm.nih.gov/pubmed/17543665
Vince D
http://www.medialapproach.com
Great pickup
Ha! Vince. I didn't even notice that. Thanks.
Dawn Altman, Admin
Hyperkalemia and DKA
I again can not thank you all enough for the excellent knowledge and wisdom that you all give with interpretation of these ECG's!!!! You all are teaching me so much, and making me love cardiology more and more each time!!
Erik Testerman, AAS, LP, NREMT-P
Patient Follow up
Just wanted to give this excellent group of clinicians, whom I plan to learn a lot from, a follow up on this patient. Last night while working, I was able to speak to the doctor who took care of this patient in the ER. I showed this to her and she told me that she thought he was not going to make it, but he actually walked out of the hospital 4 days later.
Erik Testerman, AAS, LP, NREMT-P
Thanks for the followup
We always enjoy followups. Thanks again for the great ECGs, Erik.
Dawn Altman, Admin