This is a "classic" ECG of very good quality for you to use in a classroom setting.
The Patient: A 57-year-old man who complains of a sudden onset of "sharp" chest pain while on a long bike ride. The pain does not radiate, and nothing makes it worse or better. He is pale, cool, and diaphoretic. His medical history is unknown.
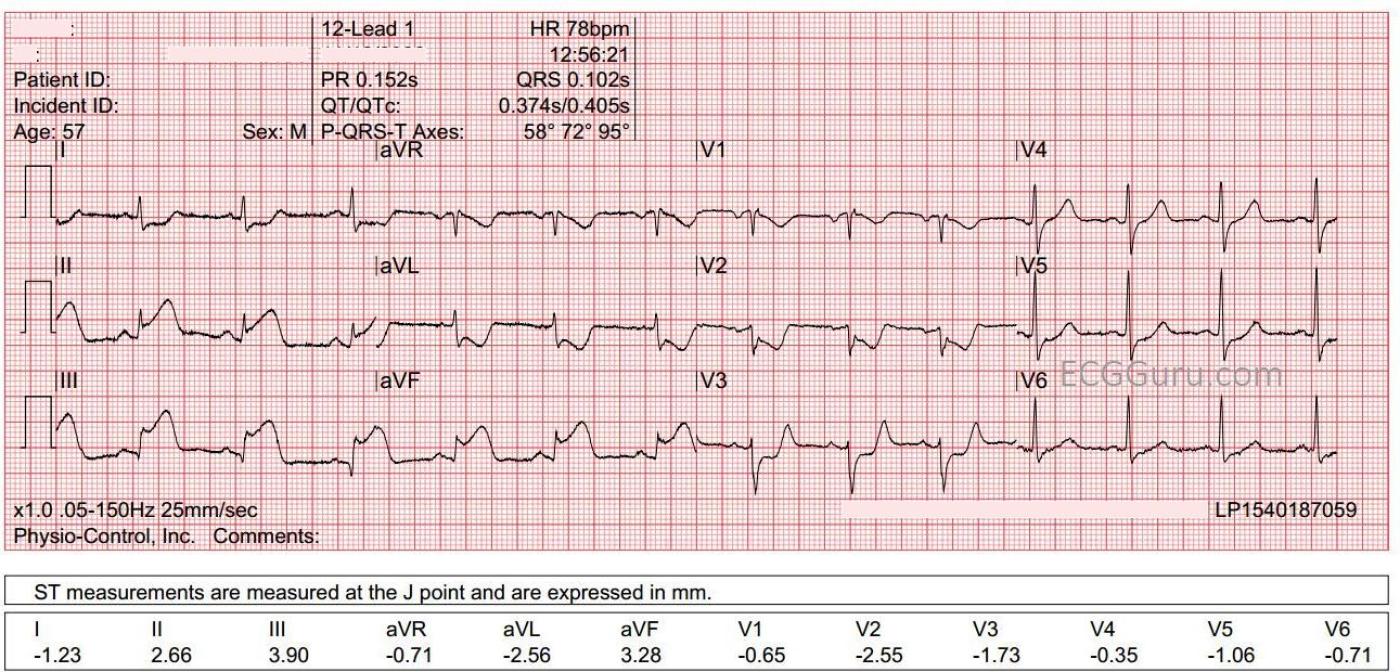
The ECG: This ECG could be considered "classic" for an inferior wall ST elevation M.I. caused by occlusion of the right coronary artery. ECG findings include:
* Normal sinus rhythm
* Marked ST elevation in Leads II, III, and aVF. The elevation is higher in Lead III than in Lead II, a reliable sign of RCA occlusion.
* Reciprocal depression in Leads aVL and I. ST depression in the setting of acute transmural ischemia (STEMI) is almost ALWAYS due to reciprocal change. The fact that this STD is localized to leads that are reciprocal to the inferior wall is proof of the nature of the STD.
* Reciprocal depression in V1 - V3. More localized depression. What wall is reciprocal to the anterior-septal wall? The posterior (postero-lateral). Since the inferior wall is really the lower part of the posterior wall, inferior wall M.I. is often accompanied by posterior wall M.I.
An additional lead, V4R, is helpful in this situation, since the right ventricle is often affected in RCA occlusions. The EMS crew reports that V4R was negative for ST elevation, but we do not have a copy.
Small q waves have formed in Lead III, and we would watch for progression of this sign, as it can indicate necrosis.
Outcome: The patient went to the cath lab, but we have no further followup.
Our thanks to Ashley Terrana for donating this tracing.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Great Teaching Example of Acute RCA Occlusion
As per Dawn — one could not ask for a better teaching example when illustrating the ECG appearance of an acute inferior STEMI! I'll add a few thoughts to Dawn's superb presentation.
While there is clearly no doubt about the diagnosis in today's tracing — I would ideally want to know a bit more about this patient's presentation. Specifically — WHEN did his CP begin with respect to the time this ECG was taken? Did this patient come in immediately? Or did the pain begin hours or a day or more before he presented to the ED? Was his course "stuttering" — or did he contact EMS immediately?
To Emphasize — Answers to these questions don't change the obvious need for immediate cath in this case — but there are many instances when they CAN affect management. The "culprit" artery will often spontaneously open (even before treatment). In fact — in many cases — there may be spontaneous reopening of the "culprit" artery — followed by "reclosure" — sometimes with repetitive spontaneous reopening and reclosure. Correlating events with the presence and relative severity of CP in association with frequent repeat ECGs may prove invaluable for telling the clinician IF the "culprit" artery is open or has reclosed (ie, If CP resolves in association with a repeat ECG that shows reduced ST elevation — then the "culprit" artery has almost certainly spontaneously reopened).
Clinically this is important — because there is often an erroneous tendency to think that IF ST elevation and CP resolve — that nothing need be done. But just because the "culprit" artery has spontaneously reopened — does NOT mean that this artery might not at any moment reclose with increased myocardial injury. This is why prompt cath with PCI is essential — even when CP has resolved.
Dawn mentioned the relatively small inferior lead Q waves. It is not commonly appreciated that: i) Infarction Q waves may form as early as 1-2 hours after the onset of symptoms (another reason for my suggestion to "hone in" on the CP history); and ii) Q waves are NOT necessarily permanent. In fact (especially if the duration of "culprit" artery closure is brief) — Q waves may sometimes completely resolve (yet another reason for "honing in" on the CP history).
As per Dawn — Looking at right-sided leads (such as V4R) is important in cases like today's case to rule out acute RV involvement. This is because patients with significant RV involvement may need IV fluids if hypotensive — and it helps to be "ready" for this by KNOWING when acute RV MI has occurred. Right-sided leads are the best way to know for certain if there has or has not been acute RV MI. That said — the finding of significant T wave inversion in lead V1 of today's tracing suggests that RV MI may be less likely (since the ST elevation of acute RV MI typically attenuates the amount of ST-T wave depression in lead V1). I'll emphasize that you should still get right-sided leads — because looking at lead V1 is not a perfect way to rule out RV MI — but in a tracing like this one — my hunch (based on the appearance of lead V1) — was NO RV MI.
On the other hand — IF on a 12-lead showing acute infero-postero MI you see slight ST elevation in lead V1 — then this strongly suggests that you DO have acute RV MI (with the ST elevation from the RV MI cancelling out what otherwise would have been more ST depression in V1 from the posterior MI).
Finally — I'll add that although a component of the ST depression in lead V2 may reflect "reciprocal change" from the acute inferior lead ST elevation — the "Mirror Test" (ie, inverting the anterior leads) — suggests that anterior leads reflect acute posterior MI by ST depression (not ST elevation).
==============================
NOTE: For those interested in more discussion and illustration of concepts that I present above — Please check out ECG Blog #387 (including the Audio Pearl and multiple links that I provided at the end of this post). This Blog #387 (https://tinyurl.com/KG-Blog-387 ) — highlights the importance of the clinical history in association with CP presence and severity with serial ECGs.
If interested in more regarding assessment for acute RV MI — Please check out ECG Blog #190 (https://tinyurl.com/KG-Blog-190 ).
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Here's a similar example
Dawn Altman, Admin