This interesting case was provided by Dr. Bojana Uzelac, Emergency Medicine physician. We are paraphrasing a translation of her comments here.
The patient is a 50-year-old complaining of chest pain.
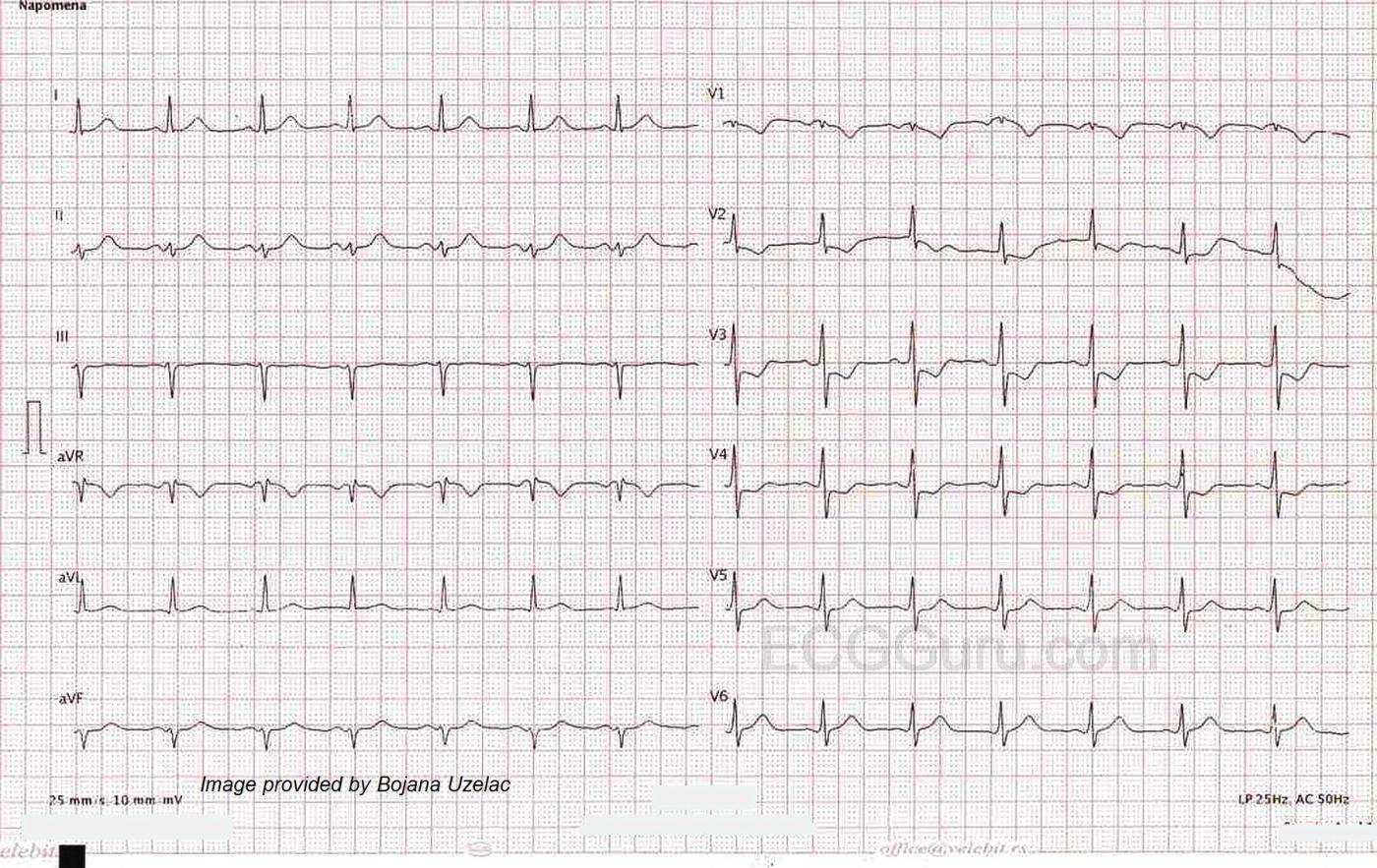
The ECG shows a rare occurrence – an isolated POSTERIOR WALL MI (PWMI). Note that leads V1 through V4 show the usual signs of posterior wall MI. We see ST segment depression, which represents a reciprocal view of the ST elevation present on the posterior wall of the left ventricle. The relatively tall, wide R waves in V2 and possibly V3 represent pathological Q waves on the posterior wall. (V2 R/S ratio > 1). What is unusual here is that there are no signs of inferior wall MI or lateral wall MI. Posterior wall MI usually occurs in conjunction with one of these.
PWMI is most often seen as an extension of inferior wall MI or lateral wall MI, because of shared blood supply. Usually, it is the right coronary artery that supplies both the posterior and inferior areas of the left ventricle (about 80% - 85% of the population). In some individuals, the circumflex artery supplies both areas. Posterior M.I. may also be seen in conjunction with lateral wall MI, when the circumflex supplies the posterior and lateral walls. In the case shown here, only the posterior wall is involved. Most cases of isolated PWMI involve either the circumflex or one of its marginal (OM) branches. Only about 3.3% - 5% of all MIs are isolated PWMI.
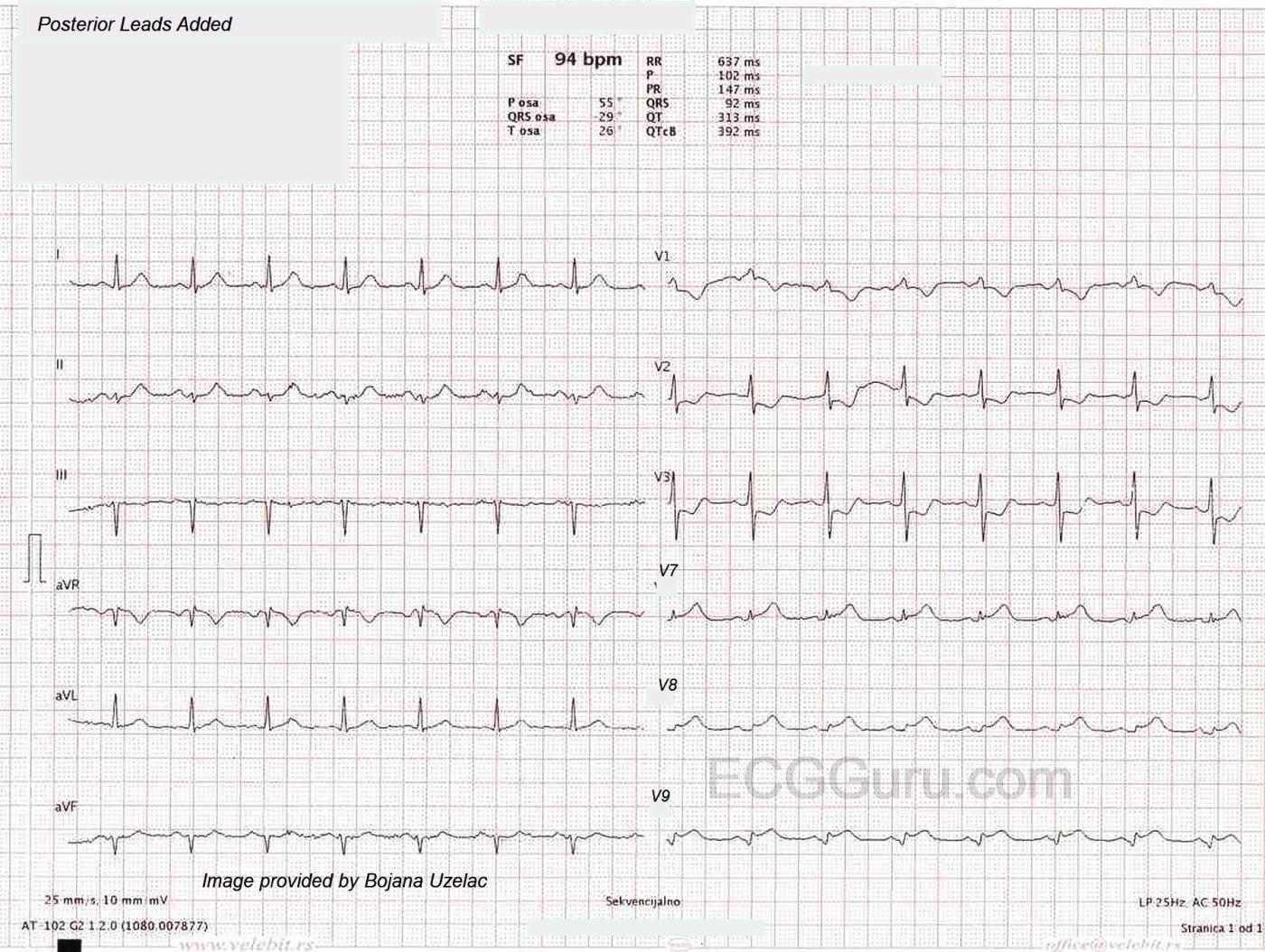
The second ECG shown here has Leads V7, V8, and V9 replacing V4 – V6. These posterior leads confirm the posterior M.I. with ST elevation. Posterior M.I. can be confirmed with STE of > .5 mm in two of the three leads. The sensitivity for this finding is not known, but specificity is almost 100%. Performance of posterior leads has been shown clinically to improve chances of recognizing IPWMI. It is generally considered to be a good idea to perform posterior leads on patients with symptoms of M.I., but no ST elevation on the standard 12-Lead ECG. For electrode placement, see HERE.
Followup The patient was taken to the cath lab, where the circumflex artery was found to be 100% occluded. The patient’s outcome was good.
Some additional resources: NIH, National Library of Medicine, Posterior myocardial infarction.
https://www.ncbi.nlm.nih.gov/books/NBK553168/
NIH, National Library of Medicine, Isolated posterior ST-elevation myocardial infarction: the necessity of routine 15-Lead electrocardiography: a case series. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9420295/
Thank to Dr. Bojana Uzelac of Serbia for sharing this important example with us. To follow her on Facebook, follow this link: https://www.facebook.com/profile.php?id=100090459765248&mibextid=ZbWKwL
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Posterior Leads Not Needed to Recognize this Posterior OMI
NOTE: When I was initially shown today's case to review — due to a technical issue, I was NOT given access to the 2nd tracing, in which leads V7,V8,V9 were substituted for V4,V5,V6. Later ( = AFTER I had written what appears below) — I was shown the posterior lead tracing. I decided to leave my initial comment — because this emphasizes a number of very important additional points that are often ignored.
TO EMPHASIZE — What follows below are VERY advanced (but important) points in ECG interpretation.
SUGGESTION — Please read KG-COMMENT #1 in the context that this is the ONLY tracing you have in front of you.
THEN — Please read KG-COMMENT #2 in the context that you are now given the 2nd tracing with posterior leads.
===========================
================
KG-COMMENT #1 (Written BEFORE I was able to see the posterior lead tracing.)
================
Interesting case of an isolated posterior OMI ( = Occlusion-based Myocardial Infarction). I will add a few additional points to the commentary by Dawn regarding this insightful contribution to the ECG Guru by Dr. Bojana Uzelac.
POINT #1 — I will respectfully disagree with the view expressed here regarding potential utility of posterior leads. In my experience over the decades since 1983 (when I first published on the utility of the Mirror Test for recognizing acute posterior MI) — I have NEVER seen an example of an ECG in which acute posterior MI diagnosed by posterior leads was not already evident in the standard 12 leads with use of the Mirror Test.
QRST amplitudes with posterior leads are reduced compared to mirror-image anterior lead amplitudes — because ECG assessment of electrical activity from posteriorly placed V7,V8,V9 electrodes has to traverse the thick back musculature before it can pick up the heart's electrical activity.
I illustrate use of the Mirror Test in my ECG Blog #317 (https://tinyurl.com/KG-Blog-317 ) — with links at the bottom of the page in Blog #317, to additional examples of how clinicians can instantly recognize acute posterior OMI by use of this mirror-image visual aid. There is no need to have to reset leads and take the extra minutes to do an additional ECG with V7,8,9 — when the history of new chest pain and applying the Mirror Test to the initial ECG can immediately provide a definitive answer.
To Emphasize: I am not against those who prefer to obtain posterior leads because they feel this helps in their interpretation. I am simply saying that with minimal practice using the Mirror Test — that equal information is obtained faster without the need to apply additional leads. (Actually — more information is obtained — since there are times when the Mirror Test is positive despite negative posterior leads).
So — In today's case, the initial ECG shows early transition with a predominantly positive QRS already by lead V2 — which as per Dawn, is sometimes insightful in suggesting posterior infarction (ie, The "reciprocal" of posterior lead Q waves may produce taller-than-expected R waves in leads V1 and/or V2). That said — it should be appreciated that lack of a predominantly tall QRS complex by lead V1 or V2 is not helpful in this differentiation — because only a minority of posterior MIs in my experience develop this sign.
But the diagnosis of posterior OMI in today's case is made principally from the downsloping ST depression in leads V2-thru-V4, being maximal in lead V3. This produces a markedly positive mirror-image (especially in lead V3) that in a patient with new chest pain, indicates need for immediate catheterization WITHOUT need to wait for either troponin values or application of posterior leads.
POINT #2 — In addition to the positive chest lead ST-T wave findings of posterior OMI that begin in lead V2 — there are 3 OTHER LEADS in this initial tracing that should immediately attract the attention of the astute emergency care provider.
The most glaring of these is lead II. In a patient with new chest pain — the flat ST segment with disproportionately tall and "fat"-at-its-peak T wave in lead II will NEVER be a "normal" finding. Even if nothing would have been seen in the chest leads — this T wave appearance in lead II in this patient with new chest pain HAS TO BE interpreted as "hyperacute".
As noted by Dawn and Dr. Uzelac — this initial ECG does not suggest associated inferior MI, because there is no ST elevation in the inferior leads. BUT — after seeing lead II — the astute clinician should realize that although the ST-T wave is completely flat (nonspecific) in lead III — the ST-T wave in lead aVF is NOT "normal". Instead — lead aVF makes for a 2nd inferior lead showing ST-T wave changes of concern, namely a flat ST segment and a T wave that looks inappropriately tall considering the small size of the QRS in this lead (and considering that one of the other inferior leads = lead II — is so obviously hyperacute). In the context of the obviously abnormal ST-T wave appearance of lead II — there should be no doubt that the ST-T wave appearance in lead aVF is also abnormal (and subtly, but nevertheless also presumably hyperacute).
Finally — My "eye" was captured by the ST-T wave appearance in lead V1. Considering how TINY the QRS in this lead is — the ST segment in V1 is inappropriately coved (much more so than neighboring lead V2) — and the T wave inversion far deeper than is usually seen in lead V1 with simple posterior infarction. I do not know the reason for this. It's possible there is some electrode lead misplacement (ie, We go from this unusual QRST appearance of the TINY complex in lead V1 — abruptly to predominantly QRS positivity by lead V2 — so I'd be sure to verify correct electrode lead positioning when repeating the ECG).
Otherwise — isolated posterior infarction is almost always a result of LCx occlusion — which essentially rules out RV involvement as a potential cause of the unusual ST-T wave morphology in lead V1. So the astute clinician should keep an eye on what happens in lead V1 as serial ECGs are obtained and the clinical situation becomes more clear.
Our THANKS again to Dr. Bojana Uzelac for this insightful contribution to the ECG Guru.
================
KG-COMMENT #2 (Written NOW THAT I AM ABLE to see the posterior lead tracing.)
================
Now that I am provided with BOTH of the ECGs in today's case — I find that the questions I raised when only having access to the initial ECG have been answered.
Did YOU realize that the posterior lead tracing was obtained some unknown time AFTER the initial 12-lead ECG? We were not told when — and we were not told whether the patient's symptoms of chest pain were the same — better — or worse.
KEY POINTS — We know the posterior lead tracing was obtained a number of minutes (or perhaps MANY minutes?) after the initial ECG — because there has been significant PROGRESSION of this evolving infarction.
— The QRS complex is now all positive in lead V1 of this 2nd tracing — and there is now J-point ST depression. This explains why lead V1 looked "unusual" to me in the initial ECG.
— Note that lead V2 in this 2nd tracing now shows much deeper ST depression than it did initially.
— Lead V3 in this 2nd tracing now shows much more terminal T wave positivity.
— We have NO IDEA of what leads V4,V5,V6 would show in this 2nd tracing — because ONLY a repeat ECG with substitution of V7,8,9 was done.
— The diagnosis of ST elevation that we now see in leads V7,8,9 is obvious. But this posterior lead tracing was clearly obtained AFTER the initial ECG — and from comparison of leads V1,V2,V3 in these 2 tracings — the diagnosis of acute posterior OMI is even more obvious now from inspection of leads V1,V2,V3 in the repeat tracing.
— There has also been progression in the limb leads in this 2nd tracing. Although subtle — the upright T waves in leads I, aVL and aVF are slightly "fatter"-at-their-peaks. I bet that IF regularly placed lateral chest leads V4,5,6 would have been done at the SAME time that posteror leads V7,8,9 were recorded — that they would show NOT "isolated" posterior OMI — but rather postero-LATERAL MI from this acute occlusion of a dominant LCx.
— The above is why lead the ST-T wave in lead II of the initial tracing was so striking to me — because it most probably was already reflecting reciprocal change from the posterolateral OMI resulting from acute occlusion of a dominant LCx.
================================
LEARNING POINTS from TODAY's CASE:
================================
— With a modicum of practice, the Mirror Test enables time-efficient and accurate recognition of posterior OMI without the need for doing posterior leads.
— For providers who find that posterior leads helps them to visualize posterior OMI — Be sure to indicate the specific amount of time that passes between the initial 12-lead ECG and the posterior lead tracing. IF your posterior lead tracing is done more than a couple of minutes later — Be sure to ALSO record leads V4,5,6 at the same time that you get posterior leads V7,8,9 (ie, Get both regular AND posterior leads).
— When reviewing tracings — Be sure to write ON the ECG indication of whether CP is still present, and if so how severe? Optimal clinical ECG interpretation is only possible if there is correlation between ECG findings with the presence and severity of CP at the time each ECG is done.
— Please consider review of my ECG Blog #351 (https://tinyurl.com/KG-Blog-351 ) for further illustration of these concepts.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
A Few More Comments on This Rare ECG...
I certainly agree with Ken that posterior leads are not necessary for a diagnosis of what we TODAY know to be a LATERAL transmural ischemia (formerly posterior MI and which I compromisingly refer to as a posterolateral MI). However, I can think of three reasons for doing them:
1. If the ST depression in Leads V1-V3/4 is very subtle and you want validation
2. If you suspect an ACS in someone who otherwise has absolutely no findings on the initial 12-lead ECG.
3. If you want physical documentation of your diagnosis, because if the ECG ever ends up in court, the plaintiff will have an expert witness who will insist that the diagnosis could have been any of a number of OTHER diagnoses based only on a single ECG.
I stopped using the Mirror Test back in the early 1970's. I found it interesting, but it never told me anything I didn't already know from looking at the ECG.
I am more interested in what the anatomy of the RCA and LCx was in this patient. The cath report just said "occlusion of the LCx" (which I think we all surmised pretty quickly). There's a reason why occlusions of the LCx (with extremely rare exceptions) result in isolated posterolateral MIs. In the RCA, the posterolateral branches are the ones that supply blood to the posterolateral (aka inferobasilar) surface of the left ventricle. If it is occluded, a posterolateral MI results. However, it is very rare for the posterolateral branch to be the only occlusion of an RCA. Most occlusions will be more proximal and will include the posterior descending artery (PDA) since the posterolateral branch takes off from the PDA at about the same point. The LCx however has its PDA as the last branch, so whether the LCx is dominant or non-dominant, it will still have a posterolateral branch.
Occlusion of two branches of the LCx can result in a posterolateral MI: the posterolateral branch and the obtuse marginal branch. The obtuse marginal is a very large branch from the LCx and it has its own anterior and posterior branches. It's those posterior branches of the obtuse marginal that feed the inferobasilar area of the left ventricle. Clarification: while there can be several marginal branches from the LCx, there can be only ONE obtuse marginal. Diagrams with EVERY marginal artery labeled as "obtuse marginal" are WRONG! There can be only ONE obtuse marginal branch.
I cannot recall EVER seeing an isolated posterolateral MI caused by an RCA occlusion. They have always been accompanied by evidence of inferior transmural ischemia. But - as I said - the LCx can produce a posterolateral MI even when it is non-dominant because - in either case - it retains both branches whose occlusion could result in such an MI.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd