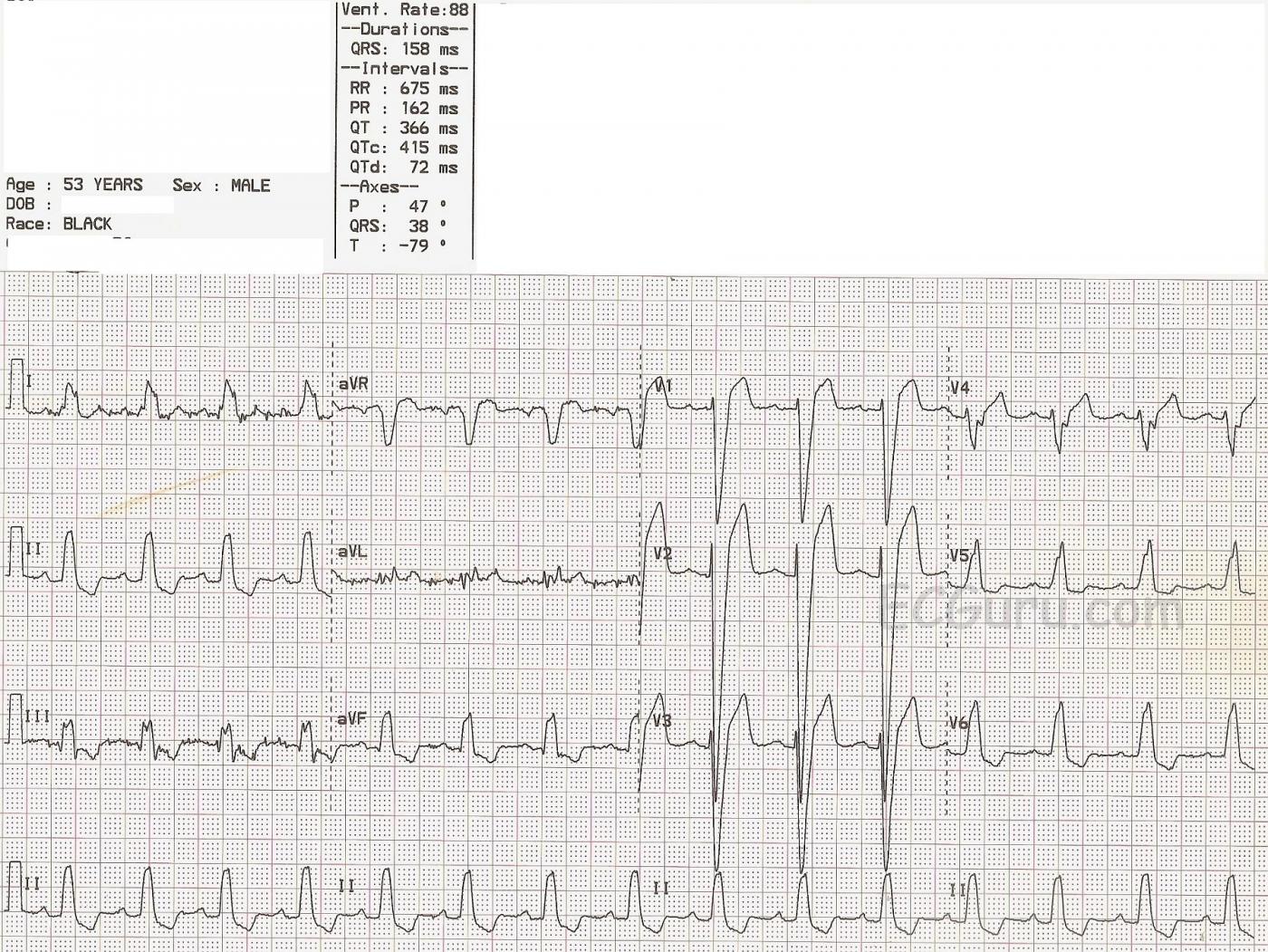
This ECG offers several teaching opportunities. First, it is an example of left bundle branch block (LBBB). It was obtained from a 53-year-old man who was undergoing a cardiac cath for chest pain. Unfortunately, we do not have access to his past medical history or the results of his cath. The ECG criteria for a diagnosis of LBBB are: 1) wide QRS complex; 2) supraventricular rhythm; 3) negative QRS in V1 and positive QRS in V6 and Lead I. This ECG shows normal sinus rhythm at a rate of 88 bpm and a wide QRS at 158 ms (.158 seconds). The QRS in V1 is negatively deflected and in V6 and Lead I it is positive.
In LBBB, as with any condition that significantly widens the QRS, there will be ST-T changes. The ST segment will deviate in the opposite direction of the QRS. In other words, there will be ST elevation in leads with negative QRS complexes and ST depression in leads with positive QRS complexes. LBBB causes significant difficulty for those trying to diagnose acute ST elevation using ECG alone. Excessive ST elevation in a lead where elevation is expected OR ST elevation in a lead where depression is expected should be considered to be abnormal. At this point, you may find it useful to review Sgarbossa's Criteria regarding determining the presence of acute M.I. in the presence of LBBB.
LBBB can be a serious functonal problem for the patient, as the slow ventricular conduction that causes the wide QRS results in less-than-optimal cardiac output. This associates LBBB with congestive heart failure, both as a cause of CHF and a result of CHF. Many people with LBBB and CHF can be helped by cardiac resynchronization therapy - pacing both ventricles synchronously to narrow the QRS and improve cardiac output. For an excellent article on cardiac pacing in general and CRT (page 2299), go to the 2013 European Society of Cardiology Guidelines as reported by the European Heart Journal, (2013) 34, 2281–2329 doi:10.1093/eurheartj/eht150
Another reason we have featured this particular ECG, is that there is significant artifact in Leads I, III, and aVL. While this artifact does not prevent us from interpreting this ECG, it is always wise to try to avoid it. In this case, it was easily remedied by replacing the left arm electrode and preparing the skin beneath the electrode by rubbing it with a dry gauze 4x4. You will know your students are learning ECG lead concepts if they can figure out on their own which electrode is the culprit in the artifact. The left arm electrode is the only one shared by these three leads, and Lead II does not use the LA.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
LBBB - Use of Modified Smith Sgarbossa Criteria
Ken Grauer, MD www.kg-ekgpress.com [email protected]