Today, we reprise an ECG originally published in 2012. We welcome comments and questions, and all questions will be answered by one of our experts.
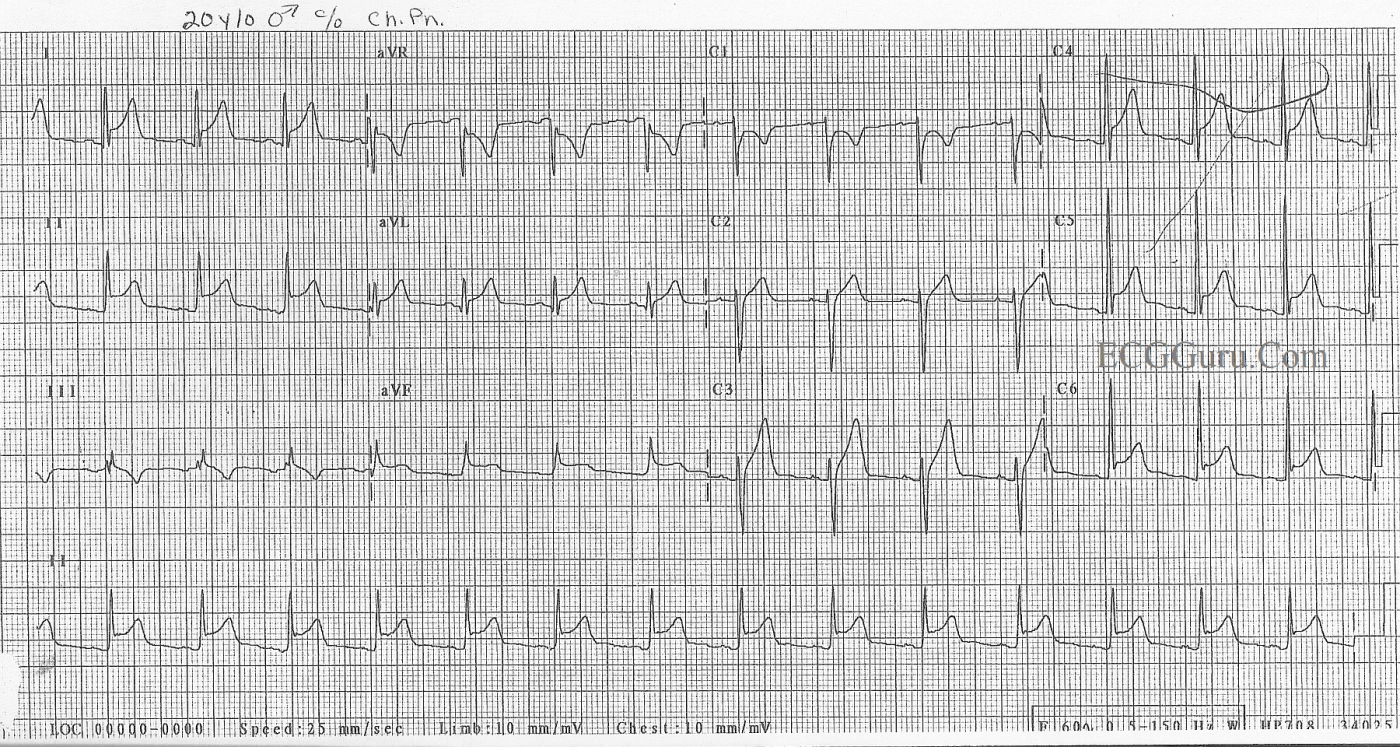
This 20-year-old man was feeling "sick", with a fever and malaise. He also complained of chest pain, which was partly relieved by sitting forward. He had a recent history of IV drug use. This ECG shows the tell tale signs of pericarditis: 1) widespread ST elevation without the other signs of M.I. He has no T wave inversions, reciprocal ST depressions, or pathological Q waves. 2) He has a subtle depression of his PR segments, which can be a difficult sign to see. 3) Spodick's Sign, a downsloping of the RP segment.
Additionally, his ST elevations are similar throughout the ECG, in height and in shape. Acute M.I. usually shows variations in the ST changes as we look closer to the center of the injury, or at the outskirts.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute Pericarditis (Not Acute MI) — in a 20yo with Chest Pain
This week’s Instructor ECG is presented as a case of Acute Pericarditis. I’ll therefore suggest that rather than try to “guess” the diagnosis (which we are immediately told) — We should use this case as a learning opportunity to review all the reasons why this diagnosis is correct.
FIRST — The history should make you suspicious of acute pericarditis even before you look at the ECG! That’s because the patient is a young adult (20yo) — who presented with positional chest pain (relieved by sitting forward) — with a recent febrile illness associated with malaise. This presentation is highly typical of acute viral pericarditis (and quite atypical for acute coronary disease). One should never say, “never” — but statistical odds are already strongly suggestive of acute pericarditis.
The ECG supports this clinical suspicion. The ventricular rate is relatively fast (close to 100/minute) — and there is diffuse J-point ST segment elevation in multiple leads. In fact, the only leads that do not show ST elevation are leads III, aVR and V1 — which are the “right-sided” leads. Even without the benefit of prior ECGs for comparision — the shape ( = upward concavity, or “smiley”-configuration) of the J-point ST elevation is highly characteristic of acute pericarditis. Q waves and the reciprocal ST depression that we expect with acute MI (Myocardial Infarction) are absent. We only see a very narrow (septal) q wave in lead aVL. The only leads with T wave inversion are right-sided leads III, aVR and V1. The pattern of upward concavity, J-point ST elevation that we see in lead II closely resembles what is seen here in lead I — whereas with acute inferior MI, it is lead III that closely resembles lead II. Finally, we have Spodick’s sign — as well as PR depression in a number of leads (leads I, II, V3,V4,V5) with PR elevation in leads aVR. While none of the above ECG findings alone are diagnostic of acute pericarditis — in the content of the above-stated history — the combination of all of these ECG signs is virtually diagnostic!
----------------------------------------------------
For those wanting Review of the ECG signs of Acute Pericarditis — Please check out Section 12.0 from my ECG-2014-ePub.
Ken Grauer, MD www.kg-ekgpress.com [email protected]