This patient is a 50-year-old man with a history of epilepsy and early dementia. He had a VP shunt placed in the hospital and was then discharged home. He became extremely weak, which was not characteristic of him, and 911 was called. He was transported to the hospital uneventfully. He was found to be afebrile.
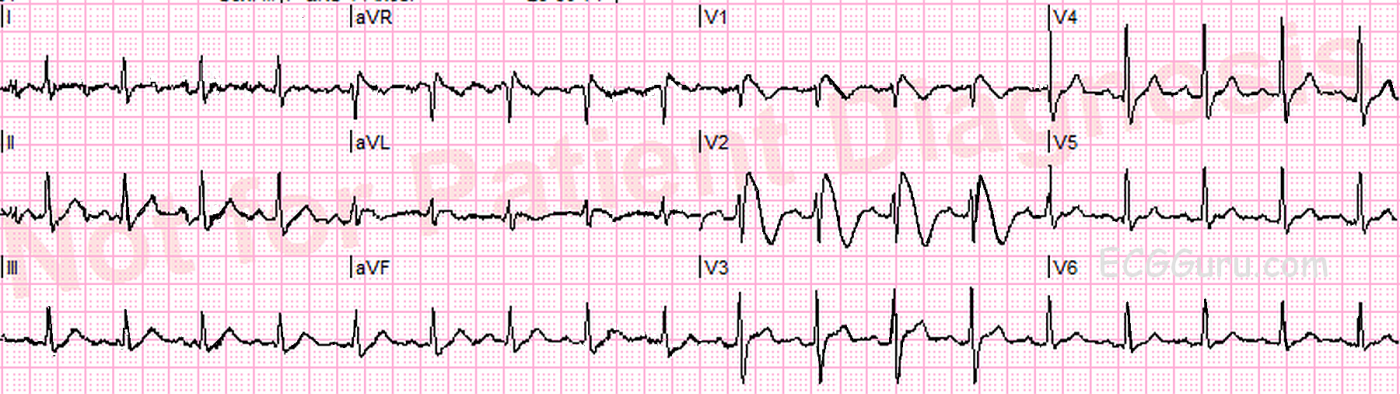
This ECG shows a “classic” Brugada pattern. Brugada Syndrome is a hereditary disease that is associated with a high risk of sudden cardiac death. It is due to a mutation in the sodium channel gene (channelopathy). The ECG characteristics are:
· ST elevation in V1 through V3 of at least 2 mm at the J point in the right precordial leads (V1-V3).
· Coved upward ST segments with negative T waves in the affected leads.
Brugada Syndrome is diagnosed when the ECG pattern exists with one of the following:
· Polymorphic ventricular tachycardia (VT).
· Documented ventricular fibrillation.
· A family history of sudden cardiac death at less than 45 years of age.
· Brugada-type ECG changes in family members.
· VT is inducible with programmed electrical stimulation.
· Syncope.
· Sleep disorders, including nocturnal agonal respiration.
Brugada Syndrome was described in 1992 by the Brugada brothers. It’s incidence is particularly high in Southeast Asia, but is a leading cause of death (after trauma) in males under 40 worldwide.
The ECG signs can come and go, and can be unmasked by multiple factors, including:
· Fever
· Ischemia
· Drugs (Na channel blockers, Ca channel blockers, alpha agonists, beta blockers, cocaine, alcohol, and others)
· Hypokalemia
· Hypothermia
· Post DC cardioversion
The definitive treatment for confirmed Brugada Syndrome is an implanted cardiac defibrillator. We do not know if the patient featured here was definitively diagnosed with Brugada Syndrome, but the ECG is an excellent example of the characteristic ST and wave changes.
Our gratitude to Palm Beach Gardens, FL, Fire Rescue Dept and Lew Steinberg for donating this tracing to the ECG Guru
References
Burns, E. (2017). Brugada Syndrome. Life In The Fast Lane. Accessed from https://www.lifeinthefastlane.com/ecg-library/brugada-syndrome/amp
Postema, P.G. (2013). Brugada Syndrome. ECGpedia. Accessed from http://en.ecgpedia.org/wiki/Brugada_Syndrome
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
An ECG Pattern to Remember (Brugada)
As per Dawn, the ECG findings seen in leads V1,V2 of this ECG are absolutely diagnostic of a Brugada-1 pattern. Depending on quality of life and advance directive issues in this patient with significant other morbidity — the next management priority would consist of EP referral for full evaluation with consideration of ICD placement.
Ken Grauer, MD www.kg-ekgpress.com [email protected]