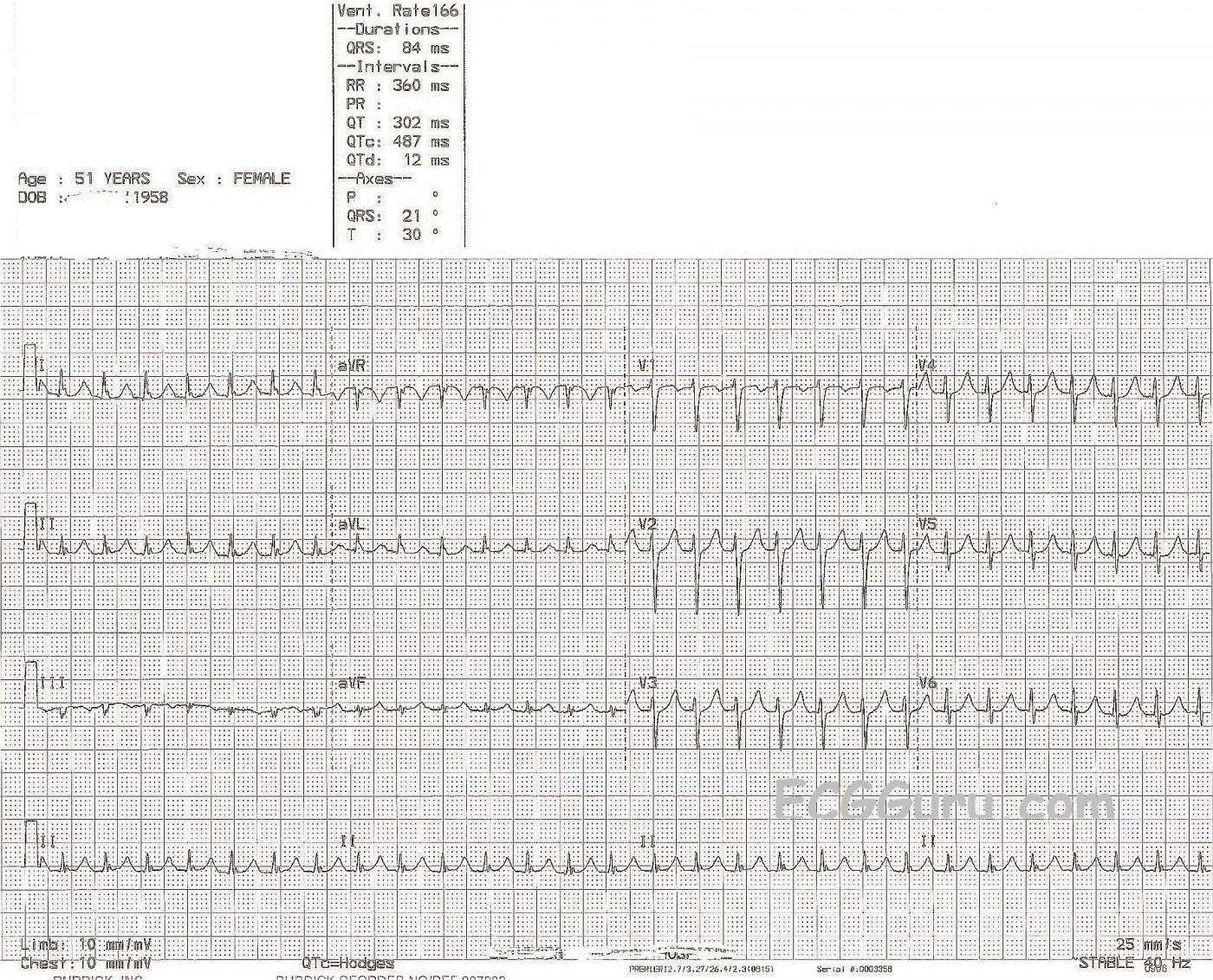
This example of supraventricular tachycardia is from a 51-year-old woman who presented to the Emergency Dept. with a complaint of palpitations. We do not have any more clinical information for her. We know this tachycardia is supraventricular because the QRS complexes are narrow. The term, "supraventricular tachycardia", or "SVT" actually describes many different rhythms with many different mechanisms and causes. It would help a great deal to see the beginning (or end) of this rhythm to determine if the onset was sudden (paroxysmal) - or gradual. Sinus rhythms tend to speed up gradually - picture a patient on a treadmill getting a faster and faster heartrate. Take the patient off the treadmill, and the rate gradually decreases. This reflects normal function of the sinus node.
SVT with paroxysmal onset indicates a re-entry mechanism, where the impulse travels from the atria to the ventricles by one pathway, but is able to return in a retrograde fashion, following a second pathway in the atria or AV node, and reenter the ventricles, depolarizing them antegradely, causing another QRS. The atria are usually depolarized retrogradely as well. Reentry can occur in the sinus node, in the AV node, or around the AV node via accessory pathways in the atria. For a very clear and concise discussion of AV nodal reentry tachycardia (AVNRT), go to this Life in the Fast Lane link. There is also a great discussion of AVNT and pre-excitation syndromes, including Wolff-Parkinson-White syndrome, at LITFL.
In this ECG, we do not know the patient's clinical situation, and we haven't seen the onset of this rhythm. The rate is 166 / min. In order for her sinus node to naturally reach this rate, we can assume she would have some visible reason for tachycardia: extreme anxiety, blood loss, hypoxia, exercise, etc. An "inappropriate" sinus tachycardia is a possibility, but not the most common thing. If she describes this rhythm as having a sudden onset, the most common and most likely diagnosis is AVNRT, also called SVT or PSVT.
The presence of retrograde P waves can aid in the diagnosis of AVNRT. Retrograde P waves are negative in Leads II, III, and aVF. They can occur before, during, or after the QRS. In this ECG, we cannot see P waves, either before or after the QRS. Some of the QRS complexes (limb leads) have a small notch at the end, but it does not look like a typical retrograde P wave in II or aVF.
If sinus tachycardia can be ruled out, it is safe to treat this rhythm with Valsalva maneuvers and adenosine, and then investigate the cause.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Don't Forget about AFlutter!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Atrial flutter?
Thanks, Dr. Ken, for your great lesson. I was troubled by the little notches at the terminal portion of the QRS, but they weren't retrograde- looking to me. I AGREE they look like hidden flutter waves! I'm usually good at catching atrial flutter, but when the rate is this fast, I sometimes miss it. (The rate is a little slow for AVNRT, but fast for atrial flutter with 2:1 conduction. Thanks for the reminder to march those flutter waves out. I wasn't there for treatment, unfortunately. Often, the true nature of the beast is uncovered during Valsalva maneuvers, carotid sinus massage, or administration of AV blocking drugs.
Dawn Altman, Admin
atrial flutter
I too wondered if this mightbe atrial flutter but I just couldn't convince myself, even after studying it closely. I'm sure the the notch on the T wave of aVL does represent atrial activity, so I wondered if the rhythm might be an atrial tachycardia with 1:1 conduction. This ECG is a great example of a SV tachyarrhythmia that is very difficult to elucidate. Sometimes, despite all the diagnostic algorithms, guidelines, tips etc that are available, it is just not possible to be sure exactly what is going on.
Dave R