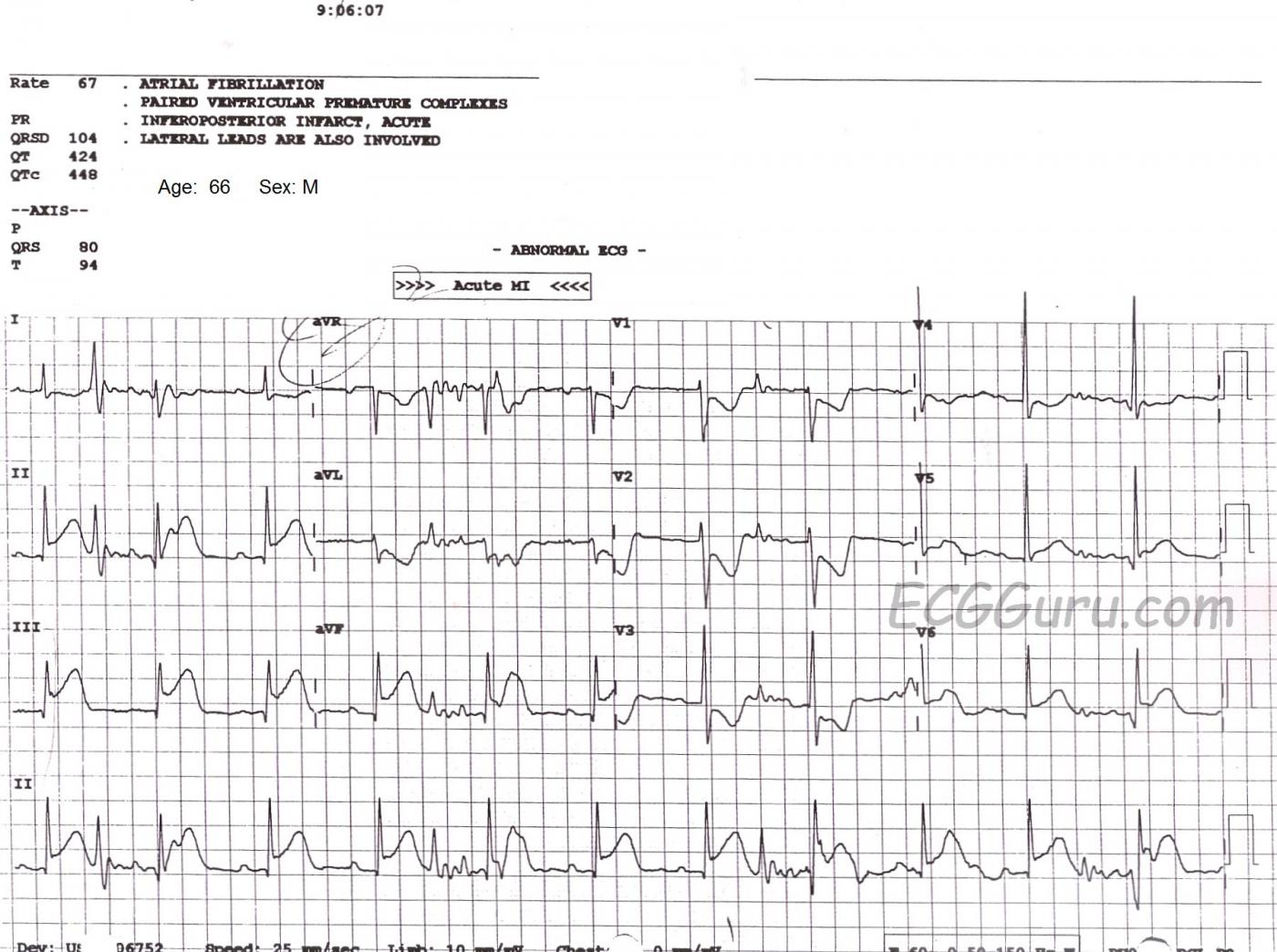
If you are an ECG instructor, it is important that you address the subject of artifact on the ECG. Artifact has many causes, and it is important eliminate it whenever possible. We should strive for the "cleanest" ECG possible. As you can see in this example, the presence of artifact has caused the machine's computer rhythm interpretation to be incorrect. The noisy baseline has caused the computer to call this rhythm "atrial fibrillation", but we clearly see P waves in all leads, especially in Lead II. We recognize these P waves as authentic because they are regular, they all look alike, and they have the same relationship to the QRS complexes each cycle (PR interval is the same).
The patient is suffering a very large M.I., showing as ST segment elevation in Leads II, III, aVF, with slight elevation in V5 and V6. In addition, Leads V1 through V3 have definite ST depression, indicating extension of the inferior wall injury up the posterior wall of the heart. There has been quite a bit of discussion lately in the literature about whether to call this a "posterior" M.I, or "high lateral", or just "inferior". Semantics aside, the involvement of so many leads tells us that this is a large M.I. The patient was in the Emergency Dept. complaining of chest pain.
It is fortunate that the artifact did not affect our ability to see the ST elevation, but it could have. And, of course, we would not want to treat this patient's "atrial fib" based on the machine interpretation. But, it is always prudent to try to get rid of artifact. In this example, Lead III has no artifact, so it could be assumed that the right arm electrode is the culprit, as Lead III does not utilize the RA electrode, and the other leads do.
Troubleshoot for the cause of the artifact, and then retake the ECG. Some common causes of baseline artifact of this nature include: patient movement, loose electrode, dried electrode, something touching the electrode, faulty or broken lead wire, and poor skin contact due to substances on the skin. The electrodes should be fresh from the package, and applied to skin that is clean and dry. The patient should be encouraged to relax and hold still (not so easy for a patient in distress). Others at the bedside should avoid touching or manipulating the limbs of the patient during acquisition of the ECG data. This only takes about 10 seconds. I have seen artifact many times when a patient's blood was being drawn during the ECG, and the patient was squeezing his fist for the phlebotomist.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute STEMI plus ARTIFACT
Excellent case by Dawn for several reasons. First — it is a good example of an acute infero-postero STEMI most probably from acute RCA occlusion (note ST elevation in lead III is clearly greater than in lead II — with marked reciprocal ST depression in lead aVL). ST elevation also appears to be present in leads V5,V6 with a hyperacute T wave in lead V6. This may occasionally be seen with RCA occlusion in which large posterolateral branches may sometimes originate from the RCA. When the cause of infero-postero MI is due to left circumflex occlusion — one usually sees ST elevation more in lead II than in lead III, and the ST elevation in V6 tends to be more than it is in lead III.
NOTE: For those wanting more on determining that the "culprit artery" with acute STEMI is likely to be the RCA (Right Coronary Artery) — Please check out my ECG Blog #80.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Filters
I agree with everything Dawn and Ken say and would just add that the reaction of many people to ECG artefact is simply to activate one or more filters on the ECG machine and repeat the recording. This may reduce the artefact but also distort the ECG waveforms; it’s much better to address the cause of the artefact directly.
Dave R