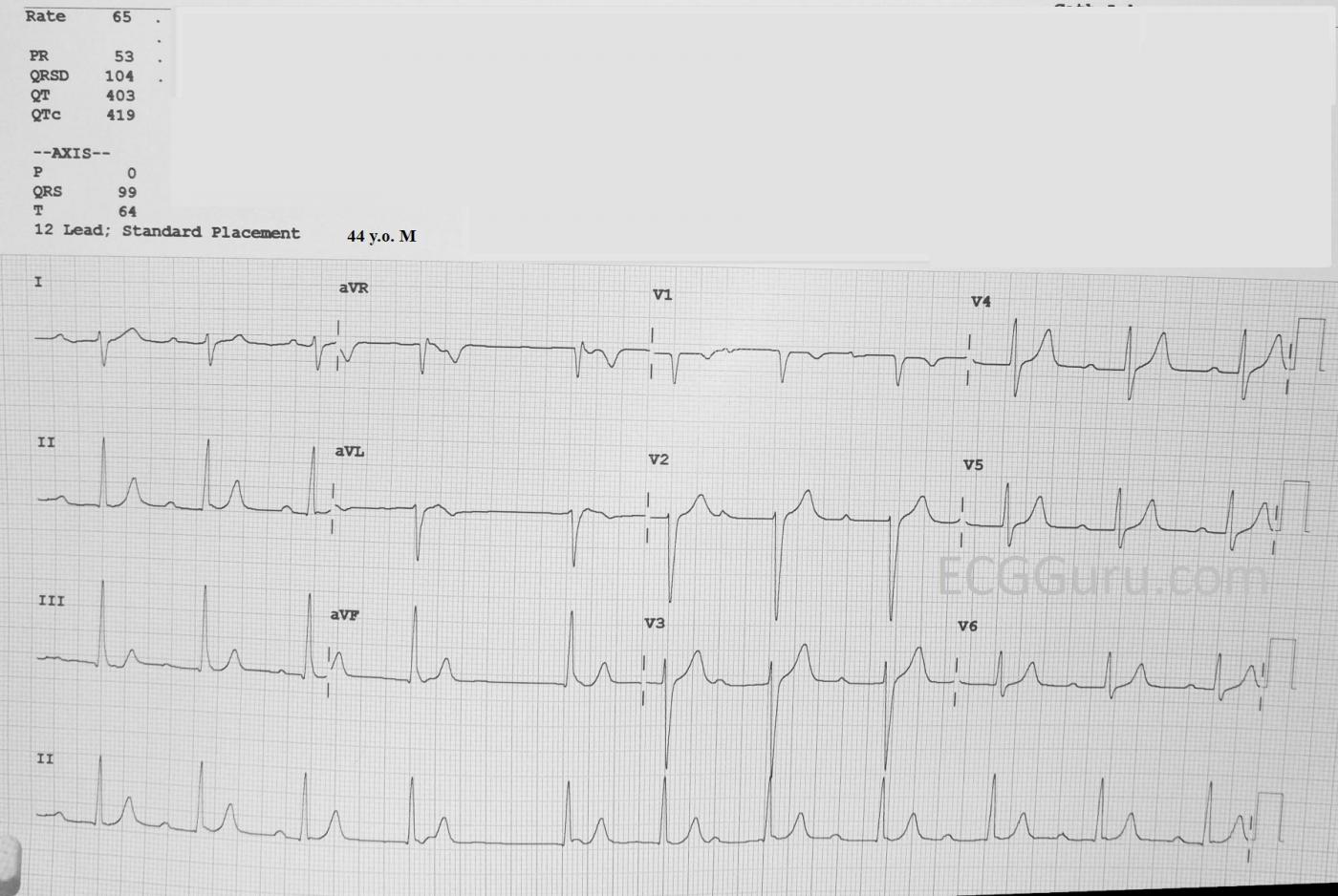
This ECG is probably not for the basic ECG interpretation class. But, it presents a challenge for the experienced ECG Gurus and instructors out there. We will leave it here for one week, to allow for comments. On June 22, we will publish Dr. Jerry Jones’s comments.
The Patient This ECG is from a 44-year-old man. He was stricken with Guillain-Barre’ Syndrome when he was 32. He doesn’t know what his ECGs showed when he was hospitalized with GBS. He knows of no abnormal lab results except for a high CK of 414, attributed to the muscle wasting with GBS.
When he was 43, he started having occasional light-headedness, and was found to have bradycardia around 50 bpm that did not increase with exercise. A loop recording showed occasional bradycardia over the next several years. This ECG is now five years old, and the patient says he no longer suffers from bradycardia or lightheadedness, only occasional palpitations and a sensation of “skipped beats”. He lives an active life, albeit with some residual lower extremity weakness from the GBS.
In order to comment on this ECG, it is necessary to “sign in” with an email address. This is so we can attempt to keep Spammers off the site. We do not use the email addresses or share them, and we will not contact you. We are looking forward to reading your comments.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Comment from Dr. Jerry W. Jones, MD, FACEP, FAAEM
This comment was sent to us via email by Dr. Jones, who is a frequent contributer to the ECG Guru and who teaches advanced ECG interpretation courses through his school, Medicus of Houston.
This is AV dissociation due to third degree AV block with sinus arrhythmia and a junctional pacemaker operating at its upper rate limit. Were there not so much parasympathetic input, we would likely be seeing an isorhythmic AV dissociation since the shortest P-P interval and shortest R-R interval are both right at 60/minute. You'll see that the P-P intervals get longer then shorter. Both changes in P-P cycle length occur (relatively) gradually. This is a reflex parasympathetic respiratory effect (via the vagus nerve) on the sinus node. The P-R intervals here get shorter and shorter, then march through the QRS. Whenever you see that happening, your first three differentials should be AV dissociation... period! Usually there is little parasympathetic influence on junctional pacemakers, but in this case there certainly appears to be some. While the P-R intervals are shortening, the P-P intervals are lengthening and the R-R intervals are also lengthening. Whenever the SA and AV nodes BOTH show the same autonomic effect simultaneously, that reflects a process outside the heart, in this case the autonomic nervous system. Then the process reverses.
There is no evidence of capture beats anywhere on this tracing, yet there are a number of P waves that should have conducted, but didn't. Don't let yourself fall into the trap of thinking that just because a P-R interval is "normal" that it must have conducted. The rhythm of the QRS complexes will tell you what is happening. If there is no 3rd degree AV block, then a capture beat will eventually occur and capture beats ALWAYS ALWAYS ALWAYS appear EARLY - never late! The early QRS will create an incongruous "jog" in the rhythm. That does not occur here. Although the rate of the junctional beats varies a bit, the only sudden change in its rhythm involves a LATE - NOT EARLY - beat. I think it is likely that the 3rd degree AV block is occuring in the AV node itself because of the narrow QRS complexes and could be transient in nature, though from the patient's statement that his doctors continue to be perplexed by it suggest that it might be permanent. A much longer rhythm strip would make me even more confident of the diagnosis. While the presence of capture beats (or fusion beats, of which there are none) rules out 3rd degree AV block, their absence does not rule it in. I am basing my diagnosis on the P waves that should have conducted but did not. That is the bottom-line, gold standard for the presence of 3rd degree AV block - NOT the presence of AV dissociation.
A big question involves the long R-R interval following the 4th QRS. I feel the parasympathetic influence reached its peak. Slowing of the rate in a sinus arrhythmia indicates that the patient is exhaling. He probably paused for a second or two before beginning to inhale again. He was probably inhaling very rapidly and then exhaling passively. A 3rd degree AV block in the AV node would preclude any reset of the junctional pacemaker.
Another issue: his T waves look a bit too symmetrical and peaked for my comfort. I would be interested to know what his BUN, creatinine and K+ was at the time the ECG was done.
Dawn Altman, Admin
Vagotonic Block — and Some (but Which?) Beats Conducting
THANK YOU Jerry for submitting this fascinating tracing. At least we agree on 2 things: i) This tracing IS fascinating; and, ii) There appears to be Vagotonic Block. Otherwise — I’ll respectfully choose to agree to disagree with your explanation.
I don’t think there is complete AV block here. I think it amazingly difficult to contemplate with any certainty which (if any) beats are conducting — let alone which beats “should conduct but don’t”. In my opinion — these conclusions cannot be confidently attained by this single tracing. I’m happy to respectfully agree to disagree with you on this.
I’m glad we agree on the likelihood of vagotonic block here. I reviewed literature on this entity when sent a tracing by a colleague. I wrote up my conclusions regarding this entity in my ECG Blog #61 — with illustration of 4 tracings on that patient. What I learned from the exercise was that AV block simply does not follow the “usual rules” for diagnosing the various forms of AV block — and recognizing this “non-follow” is the clue to suspect this diagnosis.
I respectfully submit my laddergram on your tracing. As I write on the laddergram — I truly believe some beats are conducting — but I guessed as to which beats these might be. I question how anyone can prove my theory is wrong, based on this single tracing. Many other “theories” as to which beats may or may not be conducting (including your theory!) are possible. I fully acknowledge that I do not know a definitive answer.
Thanks again Jerry for submitting this stimulating arrhythmia conundrum. Isn't it always more fun when you and I have different opinions?
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Another explanation
I’ve measured all the PP and RR intervals, as best I can, and I have shown a close-up of beats 3 and 4 for comparison of their P wave morphologies.
This is a tough one and I don’t think it’s possible to be certain what’s going on. I like Jerry Jones’s explanation but I’m troubled by the long RR interval between beats 4 & 5, then the short RR interval between beats 5 & 6. If the sudden lengthening of the RR interval is a vagal response, why is it followed immediately by the shortest RR interval in the ECG? Could a sympathetic rebound happen that quickly? And if so, why does the PP interval not shorten abruptly like the RR interval? I am also puzzled by the shape of the P wave in the ST segment of beat 4. If you look closely at the magnified view here, I think you can see that it appears to be biphasic with initial negativity, in which case it may be partially due to retrograde atrial activation and not completely of sinus node origin. So, I offer a third explanation of the rhythm, which is that that there is no AV block, just an accelerated junctional rhythm and AV dissociation simply because the sinus impulses keep encountering refractory AV nodal tissue. As the atrial rate is faster than the ventricular rate, this is not a situation that could sustain for long – a sinus impulse would eventually reach the AV node after it had recovered and then conduct. However, maybe there is sinus arrhythmia, as Jerry Jones, suggests, and maybe the 4th sinus impulse is delayed just enough to permit partial retrograde atrial activation from the junctional impulse, and maybe there are dual AV nodal pathways so that the retrograde impulse can re-enter the AV node antegradely and delay the formation of the next junctional impulse, and maybe beat 5 is a capture beat because the sinus impulse manages to conduct down to the ventricles, after which the junctional focus re-establishes control. I realise that this is an awful lot of maybes, so I am dubious of this explanation. My laddergram was very much inspired by and based on Ken’s but with an attempt to explain the apparent biphasic P wave after QRS 5, which I assume is an atrial fusion beat.
A Conundrum, Indeed!
Three experienced experts in ECG interpretation with three different explanations of the same ECG. I think it is very telling that the three of us still have some areas of agreement. It reminds me of the parable of the blind men describing an elephant.
In my reading, I have come across ECGs interpreted by Drs. Marriott and Charles Fisch, both of whom used up to three different laddergrams to describe a single ECG.
I wish we had had a longer rhythm strip in which case we might be able to see unequivocal evidence of AV conduction, but we have to use what we have. And we have to come to a conclusion based on what we have. The whole idea of doing an ECG is to help us decide what to do for the patient. In this case, I think we would all concur with the patient's previous doctors and do nothing! The patient has been doing well.
My thanks to Drs. Grauer and Richley for their very thought-provoking views of this "conundrum." In response to Ken's question at the end of his post: if we always agreed on everything, then what impetus would we have to think harder and learn more? And Dr. Richley - I've read your past posts with great interest and I enjoyed them very much. Could we perhaps hear more from you in the future?
And thanks to Dawn for a great website!
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Thank you so much, gentlemen.
I really appreciate having three of the world's best ECG instructors weigh in on this ECG. It is a fascinating tracing, and I wish we had an EP study. I have asked the patient if he possesses a long rhythm strip, which could be very illuminating. In the meantime, this is a message he recently sent me: "The bradycardia has stopped. No issue getting pulse up now. No feeling faint. However, just from pulse in neck I can feel the odd missed beat followed by a strong one. Missing maybe 1-2 per minute, lying here in bed now. I'm told it's the heart being told not to bother beating after a particular corelation of the two rhythms. Haven't had an ECG in two years (and I don't have a copy of that.)"
Dawn Altman, Admin
Civilised discussion
Thanks for your kind words, Dr Jones (and Dawn). What I particularly like about Dawn’s excellent educational site is that the discussions are serious, detailed and thoughtful and aimed at clarification rather than points-scoring. I enjoy the courteous discourse and atmosphere of civility and respect. I follow developments on ECGGuru avidly and although I am more than happy to contribute to the discussions when I feel able, after you and Ken have offered your analyses and opinions there is usually very little left to say!
GREAT Discussion!
So NICE to troubleshoot this fascinating rhythm from 3 different viewpoints! By “vagotonic block” — I would have done better to say, “excessive vagotonic influence” — since as per Dave (and as I wrote above my laddergram) — I also didn’t see any P waves that should have conducted but didn’t … — And, also as per Dave — there are “an awful lot of maybes” — and the one thing I learned from those patients that manifest this type of vagotonic “over”-infuence, is that P-P and R-R intervals defy the usual logic. What we DO all seem to agree on — is the influence of an underlying junctional rhythm (that I feel is slightly accelerated) — and what I think the 3 of us are all saying (albeit in different words) — is that excessive autonomic tone is evident. Finally, as per Jerry — I think we all agree that with a longer rhythm strip, chances are the true mechanism of this fascinating arrhythmia would be more apparent.
P.S. DAVE — You always add to the discussion !!! — :)
Ken Grauer, MD www.kg-ekgpress.com [email protected]