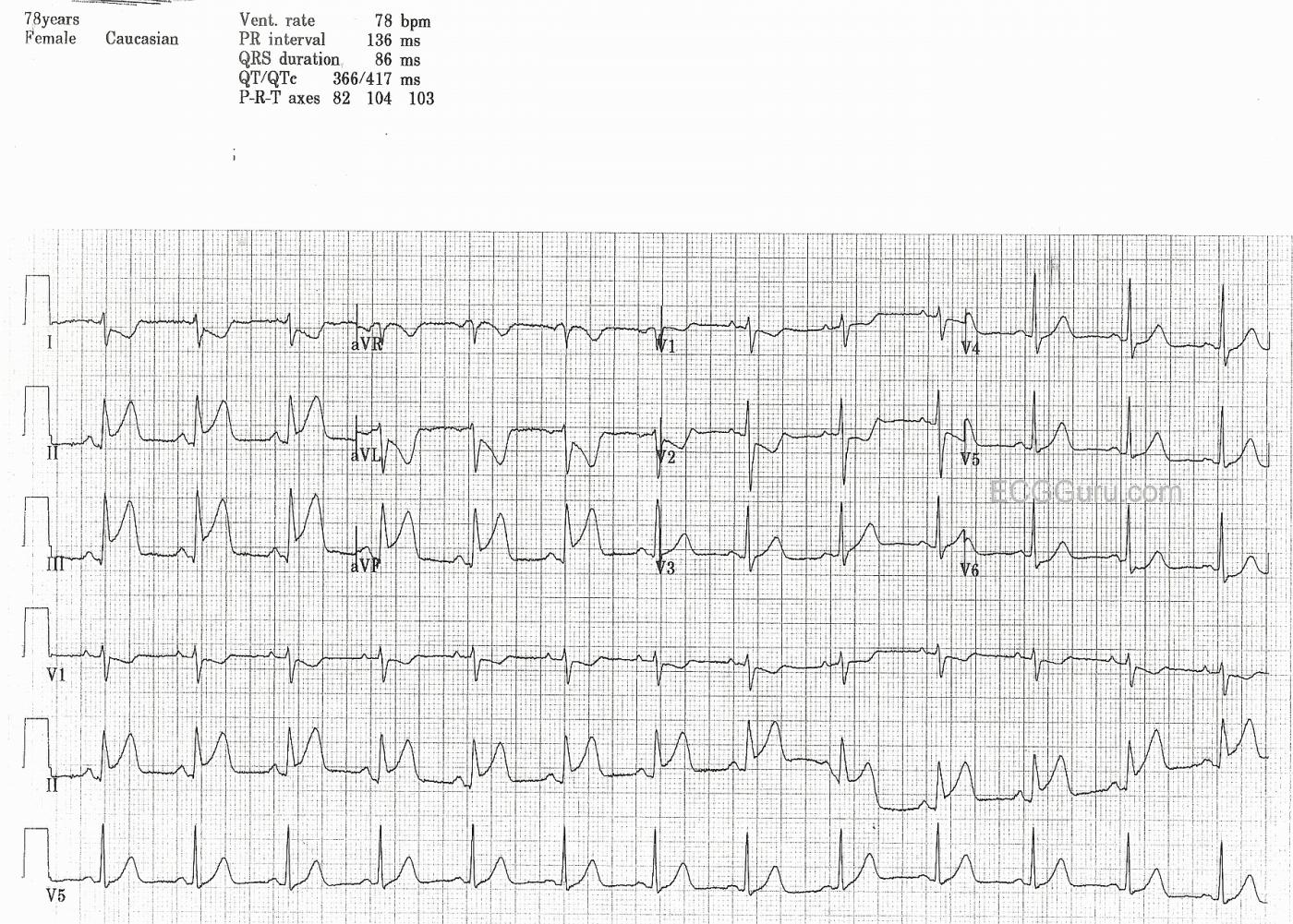
This ECG was obtained from a 78-year-old woman who had been experiencing intermittant chest pain for two days. When she finally presented to the Emergency Department, her ECG showed ST elevation in the inferior leads II, III, and aVF. She also has ST depression in I and aVL, which represents reciprocal changes seen in the high lateral leads, which are opposite the inferior wall. In addition, V1 and V2 show some ST depression, with early transition of the R waves (taller than normal for V2 and V3). This is a common finding in IWMI, and indicates posterior wall involvement. The injury is continuous from the inferior wall of the left ventricle, up the posterior wall, because both were supplied in this case by the right coronary artery.
This ECG has three rhythm strips. The more rhythm strips you have, the easier it is to determine the rhythm. In this case, the rhythm is normal sinus rhythm. But the extra rhythm strips would allow you to compare P wave morphology in three views if the rhythm was in question. Instructors: ask your students what they think about this rate (78 per minute) in the setting of acute M.I. Is it within normal range? Is it optimal for the injured heart? Another good point to bring up is the use of additional right-side leads to assess the right ventricle. V3R and V4R can be very useful in determining whether right ventricular M.I. is also present. Some practitioners skip this step and evaluate the RV using echocardiography. In the emergency setting, however, it can be very helpful to know the condition of the RV. RVMI is always a possiblity in RCA occlusion, and RVMI can increase mortality significantly. BP must be protected, since the injured right ventricle is very dependent on preload to function adequately as a pump, providing preload for the left side of the heart.
This patient was lost to followup.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
RV MI
If it is a high RCA lesion in the RCA, then yes it is RV failure. The RV marginal feeding the Right Ventricle is a vessel that originates about 1/3 to 1/2 the waydown on the RCA from the ostium of the vessel. If it is a high closure, then RV failure is inevitable. However, if the lesion is low, the RV is spared. More importantly, look at this patient clinically,If in failure, RV pressures will be high, PAWP will be low, what do his lungs tell you? and, what does is blood pressure tell you.
Susan Elwell RN, MSN - ED
Acute Infero-Postero MI from Proximal RCA Occlusion
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Is the RCA occlusion proximal?
I agree with Dawn and Ken that this an RCA occlusion, but is it necessarily proximal as Ken suggests? My understanding is that proximal occlusion is often associated with ST elevation in V1, presumably because of RV invlovement, and that ST depression in V1 suggests a more distal occlusion. Of course, I may be wrong!
Dave R
Email comment received from Dr. Adrian Baranchuk
Hi
I did enjoy your blog. The last case, however, contains some mistaken
information. The "old concept" of posterior MI (and indeed posterior wall)
due to changes in leads V1 and V2 (either ST depression or early R
transition) were removed from current guidelines, after the publications from
Bayes de Luna et al. Using MRI, Bayes de Luna convinced us that the psoterior
wall of the heart does not exists. It is inferior and basal. The old
parameters to refer to Posterior MI correspond actually to the lateral wall.
This info was collected in the latest guidelines.
However, it will take years until we change our mid set and start calling
this properly.
I have recently released an Atlas of Advanced of ECG Interpretation
(www.ecgatlas.com) that could be of interest to you, In the Atlas you will
find 100 cases described by all the ECG Masters around the world. You can
download the ECGs as PPT for your own teaching.
You will notice that I did the same mistake you did in this ECG, because I
completed the Atlas at the same time that Dr Bayes de Luna (from Barcelona,
google him or Pumed him!) was releasing this interesting concept.
Again, congratulations on a great Blog, that I will recommend to my students.
Adrian BAranchuk MD FACC FRCPC
Associate Professor of Medicine
Director, EP Training Program
Queen's University
Dawn Altman, Admin
Administrator's reply
Thank you so much, Dr. Baranchuk, for your comments. I am aware of Dr. Bayes de Luna's work (not well-versed in it). I am guilty of hanging onto the "old" ways, accidentally. It is so hard to change people's thinking. How many times have people tried to change the classification of AV blocks?
I am never offended by dissenting opinions - I am not the "ECG Guru" - the site itself is. It is meant to provide resources for ECG instructors, and your references are just such a resource. By people like yourself providing this information, the ECG Guru becomes like a "wiki" site - it constantly updates and improves. I purposely keep my comments rather simple, and rely on the comments from people like yourself for added value.
Dawn Altman, Admin
Posterior wall or not?
Dr Baranchuk makes a very interesting point. The International Society for Holter and Noninvasive Electrocardiography in 2006 (http://circ.ahajournals.org/content/114/16/1755.full?ijkey=7391a9707e270bc0a9628b266af71d6d24b48923&keytype2=tf_ipsecsha) did indeed recommend new terminology, based on MRI findings, to describe the relationship between ECG changes and location of myocardial infarction and, as Dr Baranchuk says, that group did state that there is no posterior LV wall and that the ECG changes traditionally ascribed to posterior wall MI are actually due to lateral wall infarction. However, the AHA in its 2009 recommendations for the Standardization and Interpretation of the Electrocardiogram in acute ischemia and infarction (http://circ.ahajournals.org/content/119/10/e262.full) specifically state that the recommendations of the ISHNE should not be adopted. They say, ‘It is the opinion of the committee that for the present, and not withstanding the recommendation of the International Society for Holter and Noninvasive Electrocardiography, the current ECG terminology of posterior be retained to describe ST depression in leads V1 and V2 and the subsequent development of broad R waves in these leads’.
Therefore we have two conflicting recommendations. I find it interesting that Galen Wagner was a member of both groups and a co-author of both papers!
I teach my students both sets of recommendations and try not to confuse them. This also serves the purpose of illustrating that many things in medical science are not settled, that knowledge continues to evolve and that often there are competing theories and recommendations. This is real life!
Dave R
Posterior wall as a separate entity?
My students are mostly basic-level, a few are intermediate. I have always taught them that the "posterior wall" is really just the basilar part of the inferior wall - in other words, the inferior wall faces the patient's back and left side near the base. This is variable due to position of the heart in the chest. The reason I teach it this way is that so many beginner-level students want to diagnose inferior wall M.I. AND "anterior septal wall ischemia" when they see the ST depression in V1 and V2. I am mainly trying to teach the concept of reciprocal changes, and keeping my students focused on the ST elevation, since most of my students are in the emergency field. When they see the signs of "posterior wall M.I.", they should know that the injured area is likely to be large, and the patient does not have two separate M.I.s going on. Since the LV is oval or rounded, I think it is difficult to define "walls" as separate entities. There are no corners, or even dividing lines, between the walls.
Dawn Altman, Admin