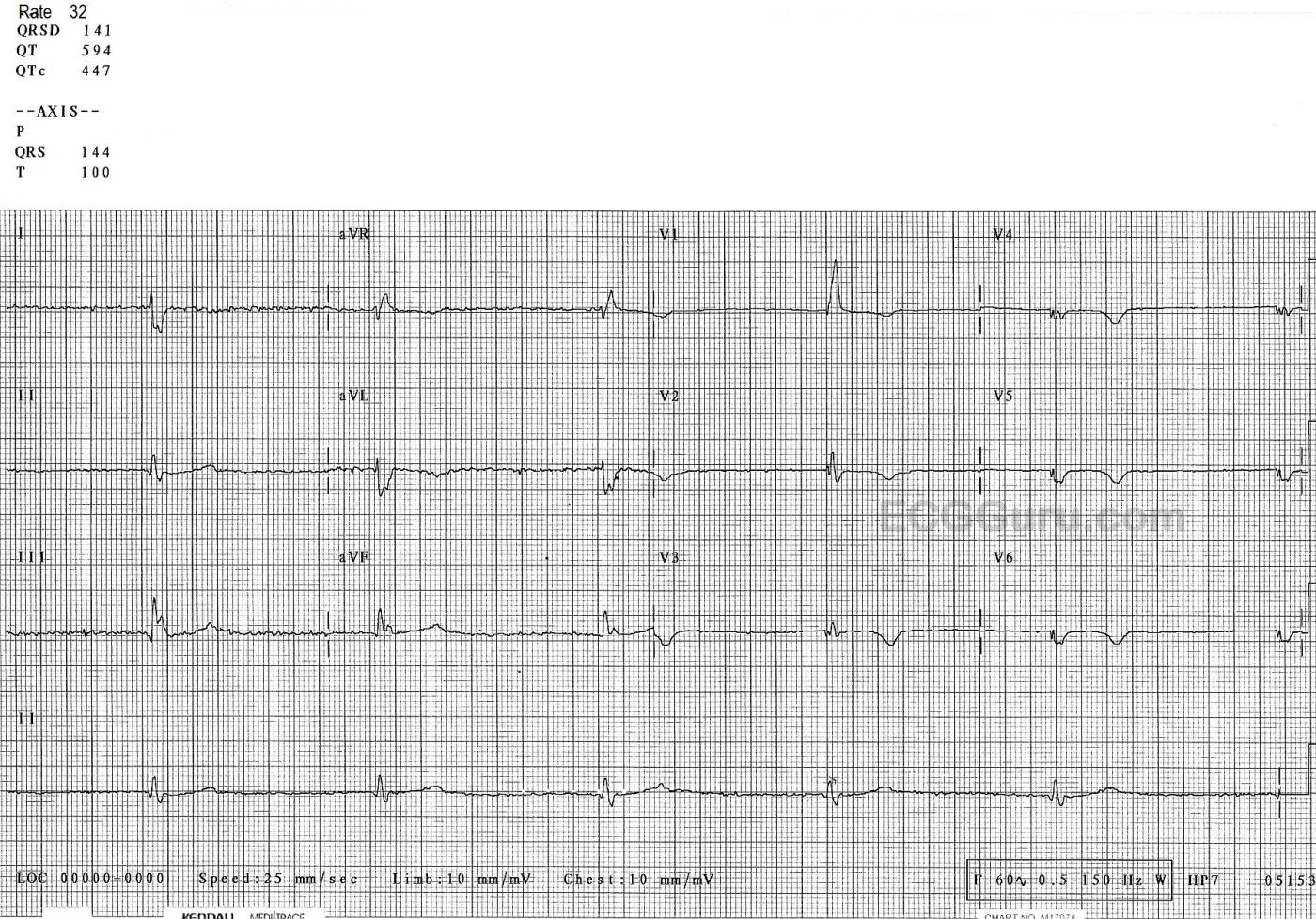
The Patient: This ECG was taken from an elderly woman. Unfortunately, we do not know any details about the case. That acknowledged, there are many interesting aspects to this ECG.
The ECG: The first thing we notice is the severe bradycardia – almost certain to be symptomatic. The rate is 32 bpm and the rhythm is regular. There are no P waves. This is a junctional rhythm, slightly slower than expected from junctional escape.
The QRS shows the presence of right bundle branch block. Each QRS on the ECG starts as a narrow complex, but then adds an “extra” wave onto the end – the delay caused by the right ventricle depolarizing late. The terminal delay is very noticeable in V1 as an R’ wave, and in Leads I and V6 as a small, wide s wave. There is right axis deviation, so the diagnosis of bifascicular block (RBBB and left posterior fascicular block) can be made.
V2 through V6 show fragmentation of the QRS complexes and a loss of voltage and R wave progression. This points to anterior wall M.I. We can’t know the age of the M.I. without clinical correlation, but the ST segments in those leads are very flat, with uniformly symmetrical inverted T waves all the way to V6. All of these signs indicate recent injury. An anterior M.I. can cause the bifascicular block we are seeing, since the bundle branches begin in the septum.
Our patient has a host of conduction system problems: there is no sign of sinus node activity, the junctional escape rhythm is slow even for the junction, there is a right bundle branch block, and the left posterior fascicle is blocked. Many diseases can cause these conduction system failures, including M.I. as well as diseases causing inflammation and fibrosis of tissues. Finding the underlying cause(s) of all these abnormalities is very important, but the FIRST consideration should be protecting perfusion by insuring an adequate rate. This patient is certainly a candidate for a pacemaker, with her bradycardia and the fact that she is living with only one main fascicle in her bundle branches (the anterior-superior fascicle).
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Slow Ischemic Fascicular Escape ...
It is always challenging having to interpret complex tracings such as this one in the absence of any clinical data. I'd add the following thoughts to Dawn's interpretation:
— i) As per Dawn — the rhythm is a fairly regular, marked bradycardia (rate ~30-35/minute). I do not see atrial activity — though assessment of this is made difficult by baseline artifact in the limb leads.
— ii) The QRS complex is obviously wide. QRS morphology is consistent with RBBB and LPHB. The unanswered question is whether this reflects a slower-than-usual junctional rhythm with bifascicular block (the usual junctional escape rate ~40-60/minute) — OR — a ventricular escape rhythm arising from the left anterior hemifascicle. I favor the latter.
— iii) Regardless of the etiology of the QRS complex — the primary problem is the marked bradycardia, which if not "fixable" — would require a pacemaker.
— iv) While it is always more difficult to assess QRS and ST-T wave morphology with non-sinus rhythms — I believe that in today's case, we still can make some deductions. There look to be small-but-present Q waves in each of the inferior leads (? inferior infarction). We only see 1 QRS complex in lead V1 — but the small-but-real Q wave in this lead suggests prior infarction. Added to this is the marked fragmenting that Dawn mentioned (probably with initial Q waves in the lateral chest leads). So while I cannot completely rule out the possibility of an escape rhythm originating from ventricular myocardium — my hunch is left anterior fascicular escape with severe underlying heart disease (suggested by all the multiphasic and fragmented complexes).
— v) Regardless of the etiology of the escape rhythm — the deep (compared to QRS amplitude) symmetric T wave inversion in all chest leads strongly suggests at-the-least, recent ischemia — and more probably, recent extensive infarction as the cause of the bradycardic escape.
— vi) While nonspecific — the very low QRS voltage in most leads on this tracing may sometimes be indication of myocardial "stunning", arising following extensive infarction. More information is of course needed — but I'd be surprised if this patient did not end up with a pacemaker.
Wish we knew more!
Ken Grauer, MD www.kg-ekgpress.com [email protected]