This ECG was obtained from a 35-year-old man who was complaining of crushing substernal chest pain which radiated down his left arm for the last ten minutes. He was diaphoretic, and described his pain as a “10” on the 1-10 scale. He got only modest relief from IV fentanyl.
He was transported to a full-service cardiac hospital, where he underwent angioplasty of simultaneous 100% occlusions of his proximal left anterior descending artery and diagonal artery. He was noted to have apical akinesia with a 35% ejection fraction.
He continued to improve following angioplasty, and was discharged home with an external defibrillator vest.
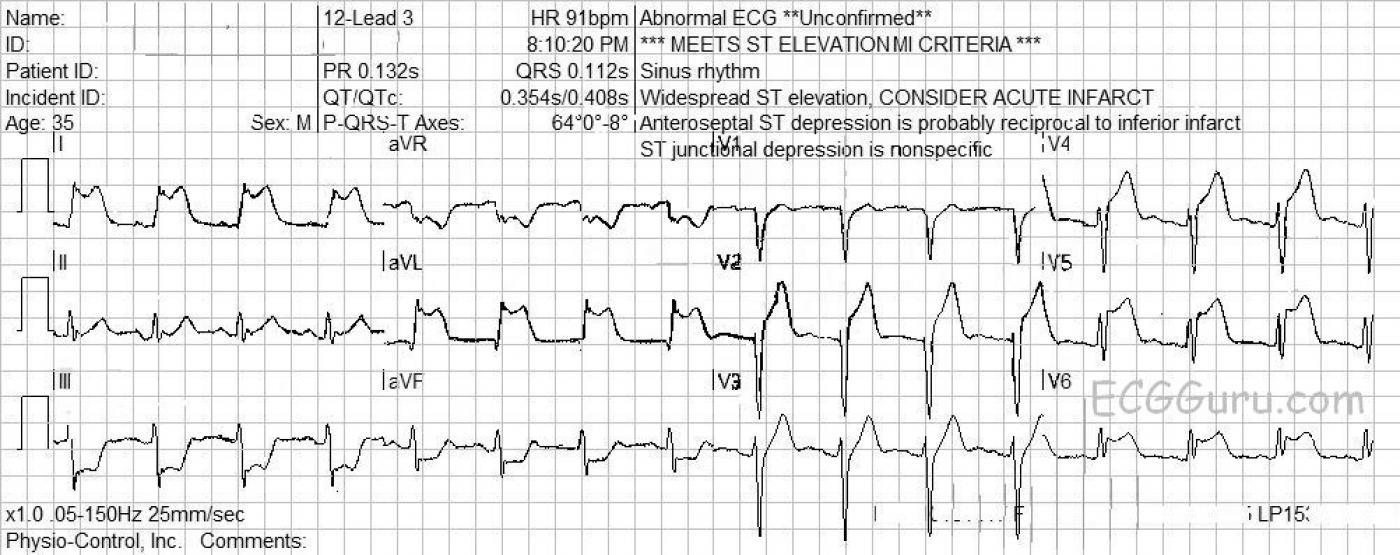
The ECG shows ST elevation in V2, V4, V5, and V6, which makes us suspect that the V2 and V3 wires were switched accidentally. This reflects damage in the anterior wall of the LV. There is also very marked ST elevation in I and aVL, reflecting damage in the high lateral wall. There is reciprocal ST depression in the inferior leads aVF and III. Fortunately, there are no pathological Q waves, which would indicate permanent damage from necrosis of the myocardium.
You can see films from his procedure in Heart Art, labeled “Simultaneous Occlusive Lesions in LAD and Diagonal”.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
I Was Surprised by the Cath Findings ...
Interesting tracing — and always nice to have cardiac cath follow-up! The occurrence of an acute STEMI with need for urgent acute cath and reperfusion in this case is obvious. What is less obvious to me is the culprit artery. Given obvious consensus on the need for acute cath — discussion about the “culprit” artery in this case is admittedly of less clinical significance, but it IS still of interest, and may be instructive.
Features atypical here (in my opinion) for acute proximal LAD occlusion are the fact that maximal ST elevation appears in the limb leads (leads I and aVL) — and that in the chest leads, the greatest amount of ST elevation is in V5. In contrast, in cases of proximal LAD occlusion — one expects maximal ST elevation in V2,V3, often with some ST elevation also in V1. So I was more suspicious of a LCx (left circumflex) acute occlusion, perhaps from a dominant LCx — than of proximal LAD occlusion. I’m not convinced that there is a lead switch (between V2 and V3) — because r wave amplitude in V3 here IS indeed greater than r wave amplitude in V2 (as it should be if the leads are correctly placed). Given that we KNOW (from the cath) there is acute 1st diagonal occlusion — perhaps that is the reason for ST elevation in lead V2 but not in V3 (Remember that isolated 1st diagonal occlusion is often manifest on ECG by ST elevation in only lead V2, but in no other chest leads).
As always — acute cath is the only way to know for certain what the anatomic lesion(s) are — and that is how we learn and hone our ECG diagnostic skills. And there ARE a number of features (ie, anatomic variants; collateralization; combined lesions) that may account for an ECG picture that doesn’t quite match what one ends up finding on cath. So, I was indeed surprised to learn of the cath results in this case = “Live & learn!”
Ken Grauer, MD www.kg-ekgpress.com [email protected]