Just like other subjects we are taught in school, ECG interpretation is usually taught in a very basic, simplistic way. As we add to our knowledge, we are able to determine the mechanisms of more complex rhythms.
When I took my first basic ECG rhythm monitoring course, I memorized all the “rules”, and at the end of the course, I thought I could read ANY strip correctly. Then, in real life, I found that some rhythms can’t be interpreted from one lead, or even from one 12-lead ECG.
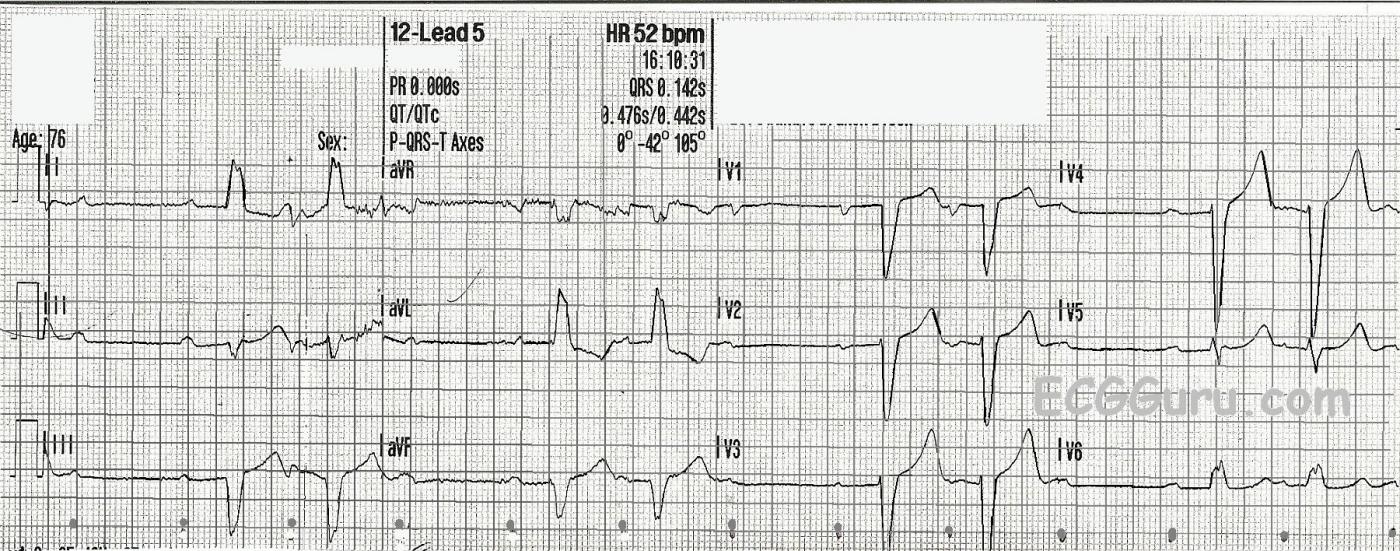
This strip offers advanced readers to challenge themselves, and it offers teachers a chance to show students an “exception to the rules” if it is appropriate for those students. We all learn the classification of second-degree AV blocks: Both Type I and Type II show an underlying sinus rhythm with some P waves conducted and some not. Type I has progressively prolonging PR intervals until a P wave is non-conducted. The cycle restarts after the dropped QRS. Type II has PR intervals that are all the same, and may be prolonged or normal.
In this ECG, you will be able to “march out” a normal sinus rhythm at a rate of 80 bpm. The P waves are marked with small dots at the bottom. Two of every three P waves are followed by QRS complexes. Is it Type I? No – the PR intervals are not prolonging. Is it Type II? The PR intervals are not the same! What is happening?
There is also left bundle branch block, which is a sub-Hisian block. Blocks occurring in the intraventricular conduction system include bundle branch blocks, second-degree AVB Type II, and third-degree AVB with ventricular escape. This group of blocks tends to be more threatening than the blocks that occur in the AV node (second-degree type I and third-degree with junctional escape).
In this strip, you will notice that the first conducted P wave in each group conducts with a PRI of about .34 seconds (340 ms). The second PRI in each group conducts with a PRI of about .24 seconds (240 ms). They are decreasing before the non-conducted beat. There are several possible explanations for the change in PRI. One is PRI alternans, due to conduction alternating through two AV pathways, one fast, one slow. Another is supernormal conduction.
We would be very interested to hear what our readers think of this interesting ECG. For beginner students – don’t be scared off by complex mechanisms. To the patient, the bottom line is RATE. Initial treatment should be aimed at maintaining a workable rate and adequate perfusion. The actual mechanism of the dysrhythmia may need to be determined later by experts, and it may require evaluation in the electrophysiology lab for a firm diagnosis.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
AV Block not following "the rules" ...
VERY interesting tracing, that as Dawn mentions doesn’t quite follow the “usual rules” we follow for assessment of AV blocks. I’d add a 3rd possible explanation to the 2 that Dawn mentions (alternating conduction through dual AV nodal pathways; supernormal conduction) — with this 3rd possibility being that may there are 2 consecutive non-conducted beats with the beat ending the relative pause reflecting junction escape that is then followed by a single conducted beat. I have no idea which of these 3 possibilities is operative (or whether there may be some other mechanism operating that I’ve not thought of ... ). What can be said, is that there appears to be severe conduction system disease. The PR interval is prolonged, and there is underlying LBBB. In addition, there are primary ST-T wave changes in at least lead V6 — which should not manifest an upright T wave with simple LBBB. Wish we had clinical follow-up on what happened to this patient!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
One of my favorite subjects...
Dawn...
Thanks so much for finding and posting this complex dysrhythmia. And I certainly agree with you about electrocardiograpy education in the US. People are given textbook examples of dysrhythmias or infarcts (some of which are drawn - not captured!) and once learned, the student feels that he or she is interpreting at an intermediate to an advanced level. WRONG!
This particular dysrhythmia exemplifies one of my favorite topics - concealed conduction. Let me tell you, when concealed conduction is a favorite topic of yours, you will see this exact dysrhythmia over and over - though in various disguises.
I have uploaded a hand-drawn laddergram of part of the lower line. Although the lower line of this ECG represents four different leads, the recording is continuous.
Let's begin with P wave #2. The PR interval that follows is most likely the true PR interval for this patient. It conducts - first down the right bundle branch and then across the septum to activate the left ventricle. The QRS interval is not all that wide for a left bundle branch block, so I would assume that the impulse crossing the septum from right to left manages to enter the left bundle branch pretty quickly rather than discharge the entire left ventricle by traveling from cell to cell.
The next P wave, P wave #3 appears too early to conduct to the ventricles. Is the block in the AV node? Maybe - maybe not. Remember: we have a pre-existing LBBB here which means the right bundle branch is initiating conduction in the ventricles. Also recall that the right bundle branch typically has a longer refractory period than the left bundle branch. In this case, however, whether the block is in the AV node or proximal right bundle branch, with a pre-existing LBBB both would look essentially the same.
P wave #3 runs into refractory tissue that is either low in the AV node or the right bundle branch and can go no further. However, its arrival there has added to the resolving refractoriness, thus prolonging it beyond what would be expected. We know this because P wave #4 encounters this refractoriness. However, due to the delay caused by the P-P interval, P wave #4 finds the lower AV node / proximal right bundle branch in its RELATIVE refractory period. Conduction is slowed and the PR interval is lengthened, but P wave #4 does manage to conduct on through. Remember that the PR interval is not just the delay in the AV node - it represents the time from the exit of the impulse from the sinus node to its arrival at the first working ventricular myocyte.
If the block is in the AV node, then it is physiologic and not necessarily life-threatening. However, if it is in the right bundle branch, there is a very serious problem here.
The prognostic value of an AV block does not lie in the DEGREE of block. The prognosis depends on the LOCATION of the block. A Mobitz I block in the infrahisian conducting system carries the same prognosis as a Mobitz II block.
I would not expect this to be a case of escape-capture bigeminy because I would expect the PR interval of the first QRS to be shorter. This would be the escape beat and it could not appear if the PR interval were normal. (If it did, it would be a fusion beat and would appear morphologically different.)
I hope this helps.
Keep up the good work, Dawn.
Jerry W. Jones, MD FACEP FAAEM
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Concealed Conduction (as per Dr. Jones)
NICE laddergram Jerry. I like your explanation! It is obvious from the underlying fragmented LBBB with primary ST-T wave changes (upright T wave in V6) — that in addition to whatever type of AV block is operative, that this patient has severe conduction disease. Given concealed conduction (as you wonderfully illustrate) — might this likely be Mobitz II (with infrahisian block) in which a beat is dropped (beat #3) after consecutively conducted complexes (beats #1,2) — with the reason why the PR intervals preceding beats #1 and 2 simply being the concealed conduction you illustrate on your laddergram? THANKS again for your laddergram and explanation!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Thanks, Ken!
Ken...
I totally agree with your thoughts about an infrahisian Mobitz II block. The only thing that creates any element of confusion here is the LBBB. It is possible that there is conduction delay in the AV node causing the concealed conduction, but it could also be due to conduction delay in the right bunde branch. I think it would take an EP study to reliably distinguish which it is. However, from a clinical viewpoint, I think I would consider it infrahisian until proved otherwise.
Jerry W. Jones, MD FACEP FAAEM
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Comments from Our Italian Colleagues
Some of our Italian colleagues have also commented (on the ECG Guru Facebook page) about this tracing. Always good to expand our discussion internationally!
Ken Grauer, MD www.kg-ekgpress.com [email protected]