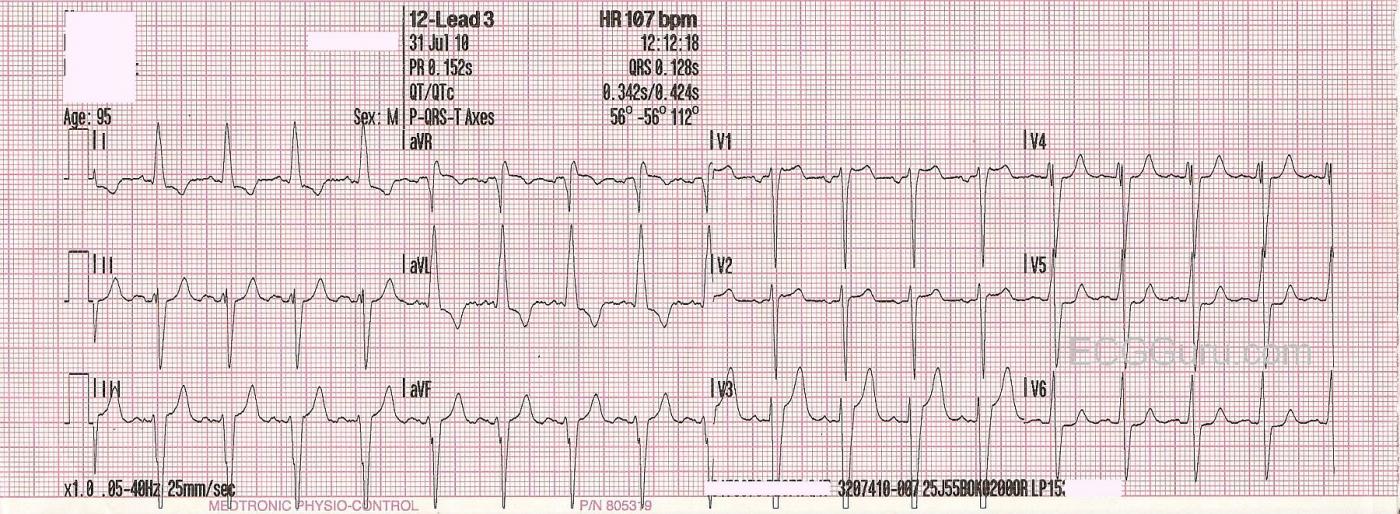
This ECG Challenge is taken from a 95-year-old man. We do not know his clinical information, except that he called 911 for assistance. We also do not have information on his past medical history. The QRS complexes are wide, and there are P waves present. What do you think the etiology of this rhythm is?
Feb. 22, 2017 UPDATE: The wide complexes in this ECG indicate an intraventricular conduction defect. The most likely IVCD at this man's age is left bundle branch block. However, the morphology of the QRS complexes in V5 and V6 are NOT typical of LBBB. Usually, there is very little or no S wave in those leads. We cannot confirm that lead placement is correct, and failing to place the left sided electrodes (V4 through V6) correctly can affect the transition of the R waves in the precordial leads. It would be SO helpful to know more about this patient, of course, but a lot is possible by age 95.
For a more in-depth look at this ECG, please refer to the Comments below.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Sinus Tachycardia with a Wide QRS Interval
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd