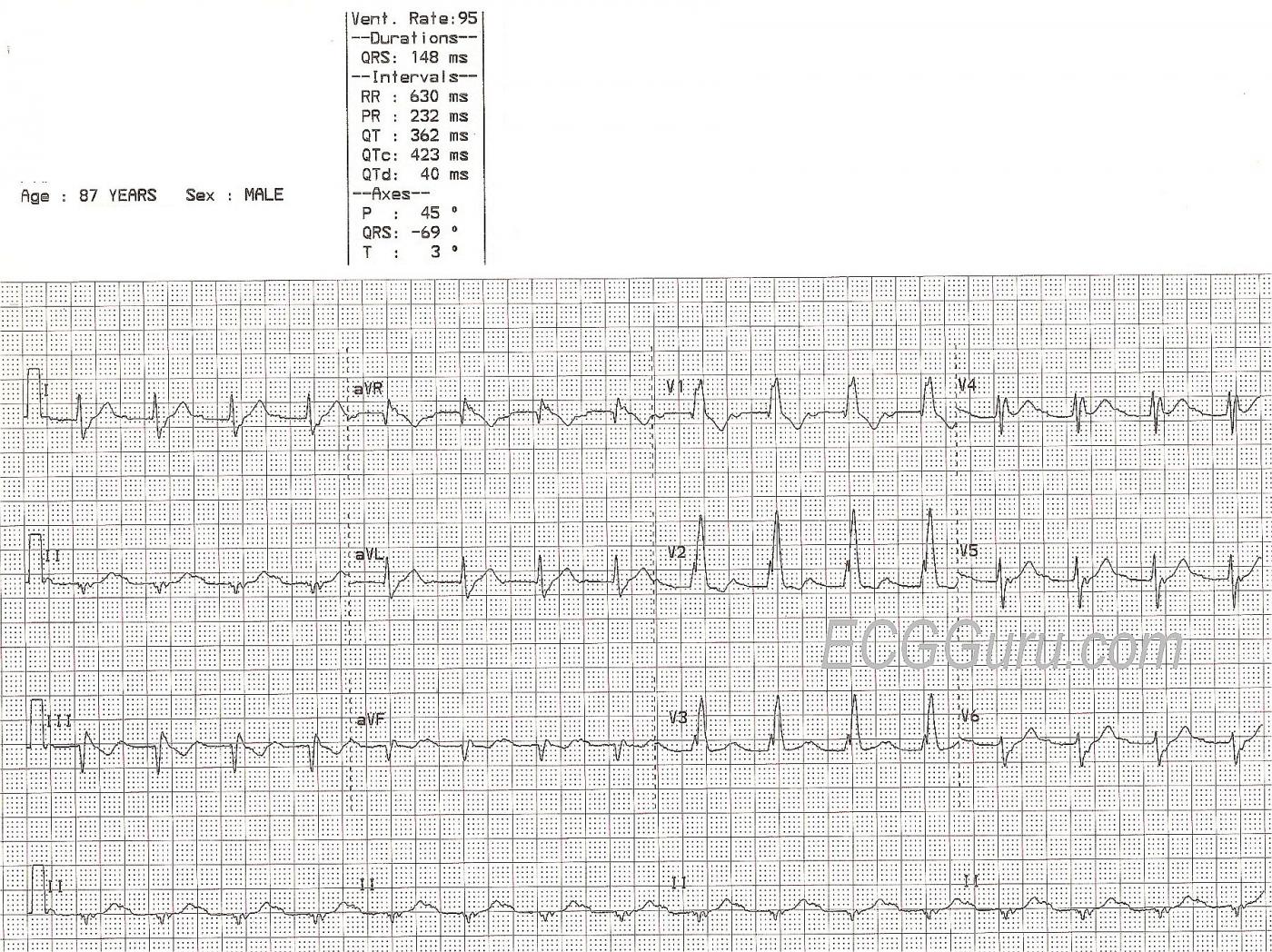
This ECG was obtained from an 87-year-old man with chest discomfort. We have no other clinical information.
ECG Interpretation The rhythm is regular and fast, with P waves, at 95 beats per minute. So, it is normal sinus rhythm, but the rate is probably not “normal” for this patient. The P waves are small, and difficult to see. We suggest Lead I to best view the P waves in this example. This is a good opportunity to teach the value of evaluating rhythm strips in more than one simultaneous lead, as subtle features may not show up well in all leads. There is a first-degree AV block, with a PR interval of 232 ms.
We see the right bundle branch block (RBBB) pattern: rSR’ in the right precordial leads (with a tiny q wave in V1, which is not typical of RBBB). The QRS is wide at 148 ms (.148 seconds). The R prime (R’) represents the right ventricle depolarizing slightly after the left ventricle. This terminal delay widens the QRS without affecting the depolarization or contraction of the left ventricle. This delay can be seen in every lead, but is especially easy to see in Leads I and V6, where there is a wide little s wave. It is normal for the T waves to be in a direction opposite that of the terminal wave (inverted in Leads V1 and III, for example.)
There is left axis deviation. The causes of LAD are many. It is not unusual for people with RBBB to also have a left anterior hemiblock (LAH), also called left anterior fascicular block. The left anterior fascicle has the same blood supply as the right bundle branch. LAH causes a frontal plane axis shift – instead of Lead II having the tallest QRS of the limb leads, Leads I and aVL will be the tallest upright QRS complexes of the six limb leads. Lead II will be very small, or flat, or negative. However, the probability of pathological Q waves in the inferior leads offers a more likely explanation for the leftward axis shift. The M.I. that would have caused these Q waves is old, as there are no acute ST changes. It would, of course, help to know this patient’s history.
Right bundle branch block can make evaluating for ST segment elevation a bit tricky. Occasionally, the terminal delay – especially in Leads III and aVF – can be mistaken for ST elevation. The J points in this ECG all appear to be at the baseline, with no overt STEMI.
Unfortunately, we do not have information about the patient’s diagnosis or outcome.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Fragmented RBBB — but Nothing Acute ...
We are told this ECG was obtained from an 87-year old man with chest discomfort. There is no additional clinical information. Dawn has reviewed most of the salient points. I’d add the following:
i) As per Dawn — it is challenging to determine the rhythm because P waves are not well seen in either lead II or lead V1. This is therefore one of the very few instances in which some other lead is looked at first. I agree that it looks like there probably are sinus P waves with a long PR interval in lead I — and it appears that this deflection in lead I does correspond to slight notching toward the end of the ST-T wave in lead II. That said, before I could be totally convinced that these are indeed sinus P waves — I would check prior tracings and attempt additional monitoring leads to try to get a better assessment of atrial activity.
ii) Assuming this is indeed sinus rhythm with 1st-degree AV block — there is also RBBB, as Dawn mentions. I’d add that there is significant “fragmentation” (ie, notching) of the QRS complex in many leads — which suggests “scarring”, either from coronary disease and/or cardiomyopathy. This is not a surprising finding in an 87-year old man.
iii) As per Dawn — the small-but-definitely-present q wave in lead V1 in this patient with RBBB is not normal. It may indicate anterior (or anteroseptal) infarction has occurred at some point in time.
iv) I agree that there appear to be Q waves in the inferior leads. Since RBBB affects terminal (but not initial) QRS depolarization — you CAN see infarction Q waves in association with RBBB. So I strongly suspect previous inferior infarction here. That said, the ST-T waves in my opinion do not suggest any acute change. Clearly, availability of a prior ECG for comparison would be helpful — but the overall appearance of ST-T wave changes here to me suggests that there is probably not any ongoing acute ischemic process.
v) As per Dawn — it is often difficult to determine if predominant negative QRS complexes in inferior leads reflects LAHB, inferior infarction, or both. That said, I would not call “LAHB” in this example — as all 3 inferior leads manifest a terminal r’ rather than rS or QS complexes that one would expect to see if there was LAHB.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
A Good Study in RBBB
Thanks to both Dawn and Ken for an excellent discussion. I would just like to add a few things about RBBB.
First, it has been my life-long task to dispel the notion of "rabbit ears." An rSR' is certainly frequently seen in RBBB but it is not seen in all cases of RBBB (as in this ECG) and not all cases of rSR' are RBBB. Here is what I need to diagnose RBBB:
1. A QRS interval duration =/> 0.12 seconds
2. A terminal R wave in V1.
3. A slurred, terminal S (or s) wave in Lead I.
4. A repolarization abnormality.
I never depend on "rabbit ears." I first learned about "rabbit ears" back when I was a med student and thought I was pretty good at diagnosing RBBB. Back then we had to do the ECGs ourselves on all our patients using a single-channel machine that produced a long strip of paper (like you see in cash registers). We recorded the limb leads first (I, II, III, aVR, aVL, aVF) and then we recorded the six precordial leads using a single suction-cup exploratory lead. Stick the cup on, record, move the cup. Stick the cup on, record, move the cup... etc. Then we would roll the ECG up so that the first lead to be seen was Lead I. I would always wait for the attending to get to V1 so I could jump in and say "Look! A right bundle branch block!" But that never happened! The attendings never had to get past Lead I before announcing a right bundle branch block. For months I thought they were all psychic!
Another issue is the direction of the repolarization abnormalities. I usually look for them to be opposite the portion of the QRS relating to the involved (blocked) ventricle.
Thanks for a great website.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd