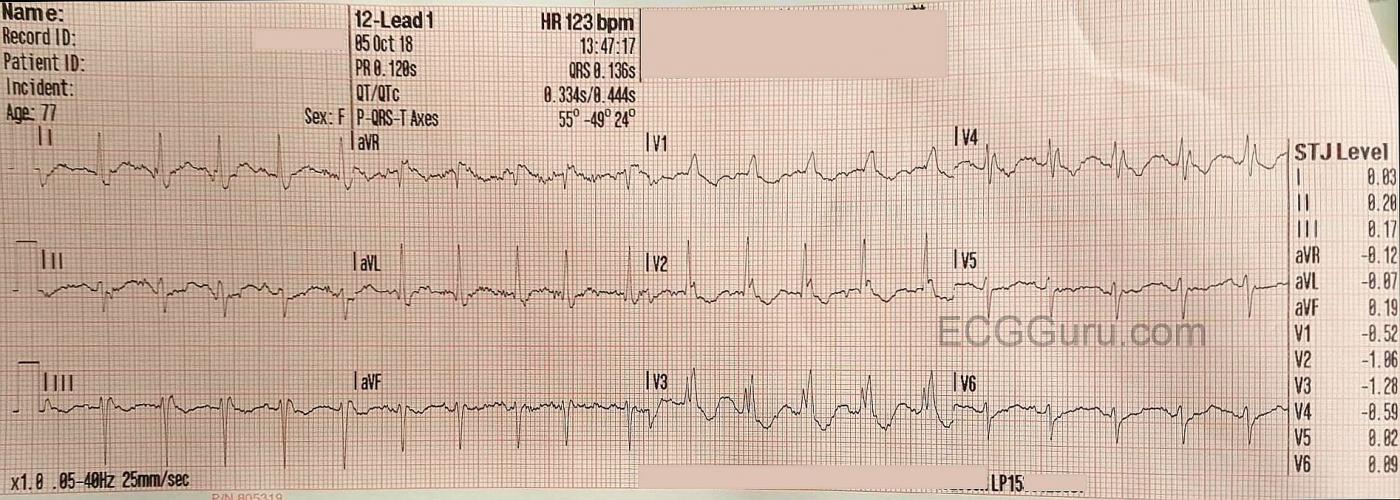
This ECG is from a 77 year old woman who was brought to the Emergency Department by EMS. She was found to be suffering from sepsis.
ECG Interpretation The ECG shows the expected sinus tachycardia at 123 beats per minute. There is significant baseline artifact, of the type usually seen with muscle tension. The artifact makes it difficult to assess P waves and PR intervals.
What we do see is RIGHT BUNDLE BRANCH BLOCK and LEFT ANTERIOR HEMIBLOCK, also called LEFT ANTERIOR FASCICULAR BLOCK. Together, these are called BIFASCICULAR BLOCK. Most people have three main fascicles in the interventricular conduction system: the right bundle branch and the two branches of the left bundle branch, the anterior-superior fascicle and the posterior-inferior fascicle. In bifascicular block, two of the three are blocked.
The ECG criteria for right bundle branch block are:
* wide QRS (> .12 seconds)
* rSR’ pattern in V1 . (the initial R wave may be hard to see, but the QRS will be predominantly upright.
* wide little S wave in Leads I and V6.
The ECG criteria for left anterior hemiblock are:
* left axis deviation ( between -45 degrees and -90 degrees)
* small q waves in Leads I and aVL
* small r waves with deep S waves in Leads II, III, and aVF.
* delayed intrinsicoid deflection in aVL (the time between the onset of the QRS and the peak of the R wave is greater than .045 seconds).
* increased voltage in the limb leads may cause aVL to meet voltage criteria for left ventricular hypertrophy, but there will be no strain pattern.
Other causes of left axis deviation should be ruled out before diagnosing left anterior hemiblock. For example, the pathological Q waves of advanced inferior wall M.I. can cause left axis deviation, as electrical forces diminish in the damaged tissue.
Most of this ECG’s J points are at or near the baseline, with some ST depression seen in V2 through V4.
Our thanks to Jonathan Hamilton for donating this ECG
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Fragmented RBBB in a Woman with Sepsis
Interesting tracing from this 77-year old woman — who presented to the ED with an acute medical problem, but apparently no chest pain. I would add the following thoughts to the comment by Dawn.
As noted — there is a lot of baseline artifact on this tracing, and this complicates assessment. That said, I believe we DO still see sinus P waves — which begin in simultaneously-recorded leads I, II and III just after the vertical RED line that I drew in parallel to the heavy grid line (See attached Figure below). When it is difficult to see P waves — use of simultaneously-recorded leads may be invaluable for confirming that deflections suspected as atrial activity do in fact occur at the same instant in time in several leads. Thus, the rhythm is sinus tachycardia.
As per Dawn — there is RBBB (Right Bundle Branch Block). Although in theory, a triphasic (rSR’) pattern should be seen in lead V1 with RBBB — many factors (ie, infarction; scarring from cardiomyopathy; chamber enlargement) may contribute to altering the nature and sequence of depolarization forces with this conduction block. Normally, the QRS complex is predominantly negative in V1. If in association with a supraventricular rhythm — there is QRS widening with an upright complex in lead V1 in association with wide, terminal S waves in lateral leads I and V6 — then RBBB may be present despite the absence of a distinct triphasic pattern in V1. This is the case in the Figure.
The concept of “axis” in the setting of RBBB is problematic. Calculation of axis is based on the average direction of the heart’s electrical activity in the frontal plane. In the presence of RBBB — electrical activity first goes left-to-right (as the septum is depolarized) — then right-to-left (as the left ventricle is depolarized) — and then left-to-right again as the blocked right ventricle is finally activated via slow myocardial conduction through nonspecialized fibers. So, in the setting of RBBB — the “average direction” of the heart’s electrical activity does not reflect the actual zig-zag path of the depolarization impulse. BOTTOM LINE: Don’t worry about “axis” when there is RBBB. All we care about when there is RBBB is which of these 3 possible settings is operative: i) RBBB and nothing else; ii) RBBB plus LAHB (Left Anterior HemiBlock); or, iii) RBBB plus LPHB (Left Posterior HemiBlock). In this case — the predominantly negative QRS complex in the inferior leads tells us there is RBBB/LAHB (= bifascicular block).
In addition to RBBB — there are 2 Q waves that should be noted. The small-but-definitely-present Q wave in lead V2 (within the BLUE circle) should not normally be present when there is RBBB. This means that in addition to RBBB, it is possible there has been prior anterior infarction. Then, in lead aVL — the Q wave in this lead is a bit larger (and wider) than is usually expected. This could be reflective of prior lateral infarction, though I can’t rule out that this might also be a normal septal Q wave. That said, the ST-T wave depression in leads V1-thru-V4 is potentially consistent with RBBB. I see some nonspecific ST-T wave abnormalities— but these do not look to be acute. I suspect they will diminish once the patient’s underlying medical condition (and her resultant sinus tachycardia) are controlled.
Finally — there is much fragmentation of the QRS complex in this tracing. By this I mean the very prominent notching in leads V2, V3 and V4. Although a nonspecific sign — excessive fragmentation of the QRS complex often signals “scarring” that may reflect prior infarction and/or cardiomyopathy.
=====================
NOTE: For more on Hemiblocks with RBBB — CLICK HERE (Begin with Section 07.17).
— For more on ECG Diagnosis of BBBs — CLICK HERE — and/or check out my 17-minute ECG VIDEO on the Basics of BBB —
=====================
Ken Grauer, MD www.kg-ekgpress.com [email protected]