The Patient: Paramedics were summoned to the home of a 74-year-old woman who had a complaint of shortness of breath. She was found sitting, alert and oriented, with labored respirations at 30/min. She stated that the shortness of breath came on suddenly. She denied any cardiac or pulmonary medical history, and said she took no medications. The patient was ambulatory. Her skin was cool and moist. Her SpO2 on room air was 85%, improving to 90% on oxygen via 15 lpm non-rebreather mask. Her lungs sounded clear.
When the patient was moved to the transport vehicle, she suddenly became nonverbal, with a leftward gaze. Her pupils were noted to be unequal and non-reactive (we do not know which was larger). Her BP was 67/43.
During transport, her heart rate declined into the 20’s and became apneic and pulseless. Recorded BP was 46/25. CPR was done until and after arrival at the hospital, where efforts to resuscitate were halted after some time.
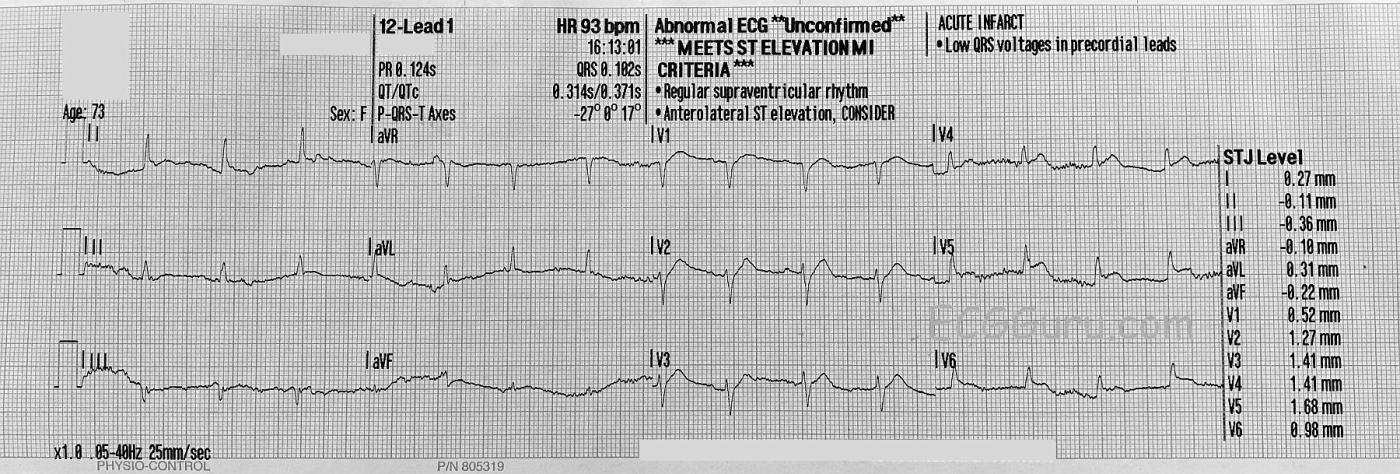
ECG Number 1: The first ECG, shown here, was taken approximately 8 minutes after arrival of EMS. There is significant artifact, making it difficult to comment with certainty on the QRS width, P waves, and J points. P waves are best viewed in the right-sided chest leads, V1 through V3. The QRS morphology appears normal and the intervals are within normal ranges.
The ST segments appear to be elevated in V2 through V5, and the machine’s interpretation confirms this (although the artifact can make measurement difficult for the machine also). In addition to J point elevation, the SHAPE of the ST segments in the precordial leads is abnormal –straightening and losing the “smile” shape that is normal. There is some mild ST depression in Lead III.
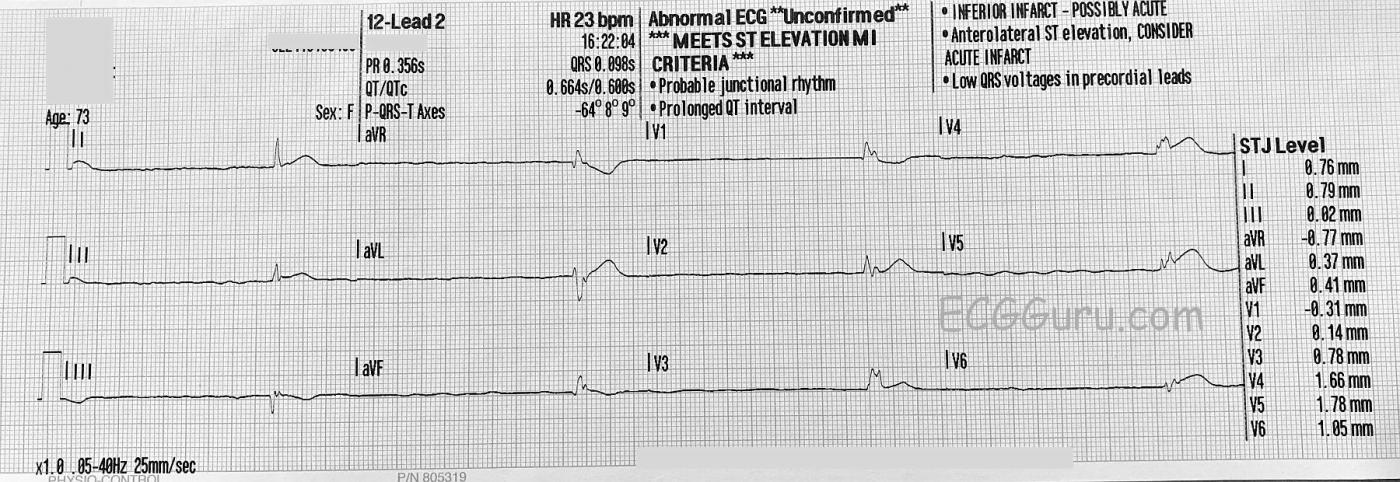
ECG Number 2: The second ECG, performed about nine minutes later, shows what happened when the patient’s condition suddenly declined. Her heart rate declined to about 20 bpm, and she was pulseless. Keeping in mind that the three channels of this 12-lead ECG are run simultaneously. So, Leads I, II, and III are recorded together, and the QRS morphology matches that of ECG No. 1. Then, when aVR, aVL, and aVF are recorded, the QRS morphology changes and becomes wider at around .12 seconds (120 ms) or more. This represents an “escape” rhythm. Even though the ECG machine records an axis for the P wave, and a PR interval, P waves appear very flat in the first 3 seconds of the ECG, and non-existent in the rest of the leads.
Assessment: It is obvious that an acute catastrophic event happened to this patient. Because she died before definitive tests could be performed, we will never know what it was. The ECG signs of ST elevation and failure of the primary pacemaker certainly fall within the realm of acute myocardial infarction, but the only symptom initially was shortness of breath, which would be a possible, but atypical, presentation. She also exhibited some clinical signs of many other life-threatening illnesses, such as stroke or pulmonary embolism, but without “typical” ECG changes.
In retrospect, we are left wondering if an M.I. caused loss of perfusion, which led to the other symptoms, or if another condition lowered perfusion, causing STEMI signs on the ECG. The common denominator here is perfusion, and our goal should be to restore perfusion in order to gain time to find and treat the culprit disorder. Depending upon the setting we operate in, we might use I.V. fluids, temporary transvenous or transcutaneous pacing, mechanical ventilation, drugs, or chest compressions to try to maintain perfusion to the brain and coronary arteries. Of course, some catastrophic medical events are just that – catastrophic – and, sadly, our efforts fail.
Our thanks to Lt. Vincent Levin for donating these ECGs.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Why Did this Patient Die? (What about the QTc?)
Unfortunate case of this previously healthy 74-year-old woman — who presented with shortness of breath, followed by a rapid downhill course. The initial 12-lead ECG shows a fairly (but-not-completely) regular, supraventricular rhythm at ~90/minute, with P waves best seen in the anterior chest leads. Artifact precludes a definitive conclusion about the rhythm — but I don’t see P waves in the limb leads. Presumably this is either sinus rhythm (with very low amplitude P waves in lead II that are hidden by artifact), or a low atrial rhythm — though further monitoring with less artifact would be needed to know for certain. As per Dawn, there is ST elevation in a number of chest leads — but not nearly as much as I would expect if the cause of this patient’s sudden demise was an acute cardiac event … There are no reciprocal changes — and ST-T wave abnormalities in leads V1-thru-V4 are primarily in shape rather than frank ST elevation. So the reason for this patient’s abrupt deterioration is not clear from her initial ECG — and non-cardiac etiologies should be entertained.
Regarding the 2nd ECG — Astute observation by Dawn (!) that QRS morphology for the first 3 leads recorded (leads I, II, III) is identical to that seen in the initial ECG. This is followed by QRS widening and a change in morphology, representing a lower escape focus with an escape rate in the 20s. No P waves are seen.
NOTE: There IS one additional finding that might be highly relevant — namely, that there appears to a short QTc interval in the 1st ECG. While definite guidelines exist for identifying QTc prolongation — it is often much more difficult to detect the far less common shortening of the QTc interval, especially when the heart rate is relatively fast as it is in this case. But the peak of the ST segments in leads V1-thru-V5 clearly appears to occur sooner-than-it-normally-does. The most important clinical condition associated with QTc interval shortening is hypercalcemia. In my experience — fairly marked serum calcium elevation is usually needed (ie, >12 mg/dL) before ECG evidence of QTc shortening is detectable. Realizing that we have NO additional clinical information on this case — I will venture ahead with a potential scenario that might account for the sudden CNS deterioration that this patient seemed to experience = Perhaps she had marked hypercalcemia from a terminal malignant condition with cerebral metastases … Unfortunately, we will never know.
FINAL THOUGHT: The pre-terminal ECG will not always tell us the cause of a sudden clinical demise. That said, it is good to keep in mind that clinical correlation, in light of ECG findings — may at times suggest a possible non-cardiac cause.
------------------------------------------
Relevant to This Case: Please check out my ECG Blog #54 — in which the acute ST elevation on the ECG was not due to a STEMI, but rather to Hypercalcemia!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Perplexing!
Great analyses by Dawn and Dr. Grauer. I don't have much to add except to speculate that the MI may have been much larger than just an anterolateral MI. I suspect that this may represent an occlusion of a wrap-around LAD just proximal to D1. We see STE in V2 - V6 in the precordial leads (maybe even a little bit in V1, too) and STE in Lead I. However, there is no STE in aVL and the inferior leads are not clearly seen. There is a lot of baseline wander and artifact. In at least one QRS in both Leads II and aVF there may be a suggestion of early or perhaps mild STE but nothing in Lead III. Which brings us back to the location of the LAD occlusion. If V2 is involved then surely the occlusion is proximal to D1 which should also cause STE in Leads I AND aVL. But we have no STE in aVL when there probably should be STE in that lead. And no STE in Lead III. I think there is STE in both aVL and Lead III but they have cancelled each other out. I have seen cancellation of forces of this type also have a profound effect on on the ST segments of Leads II and aVF in addition to Lead III.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd