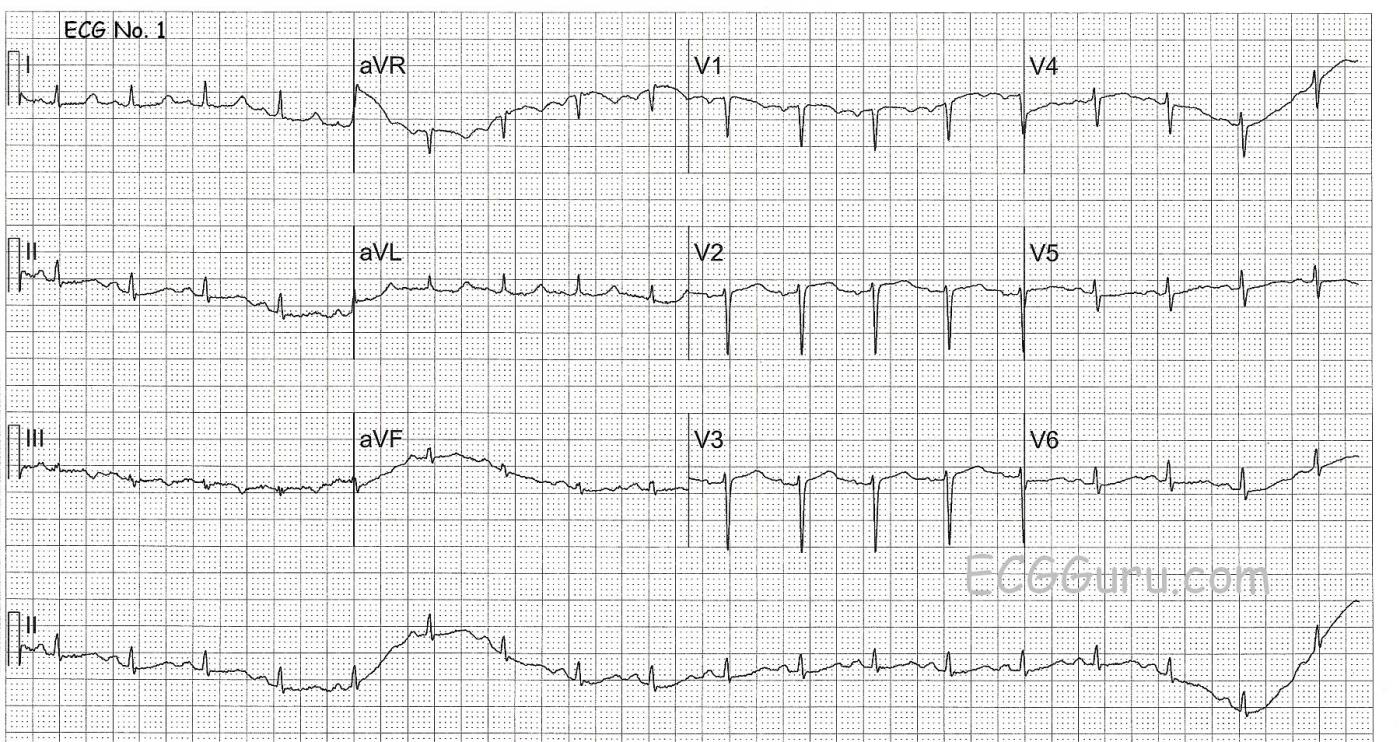
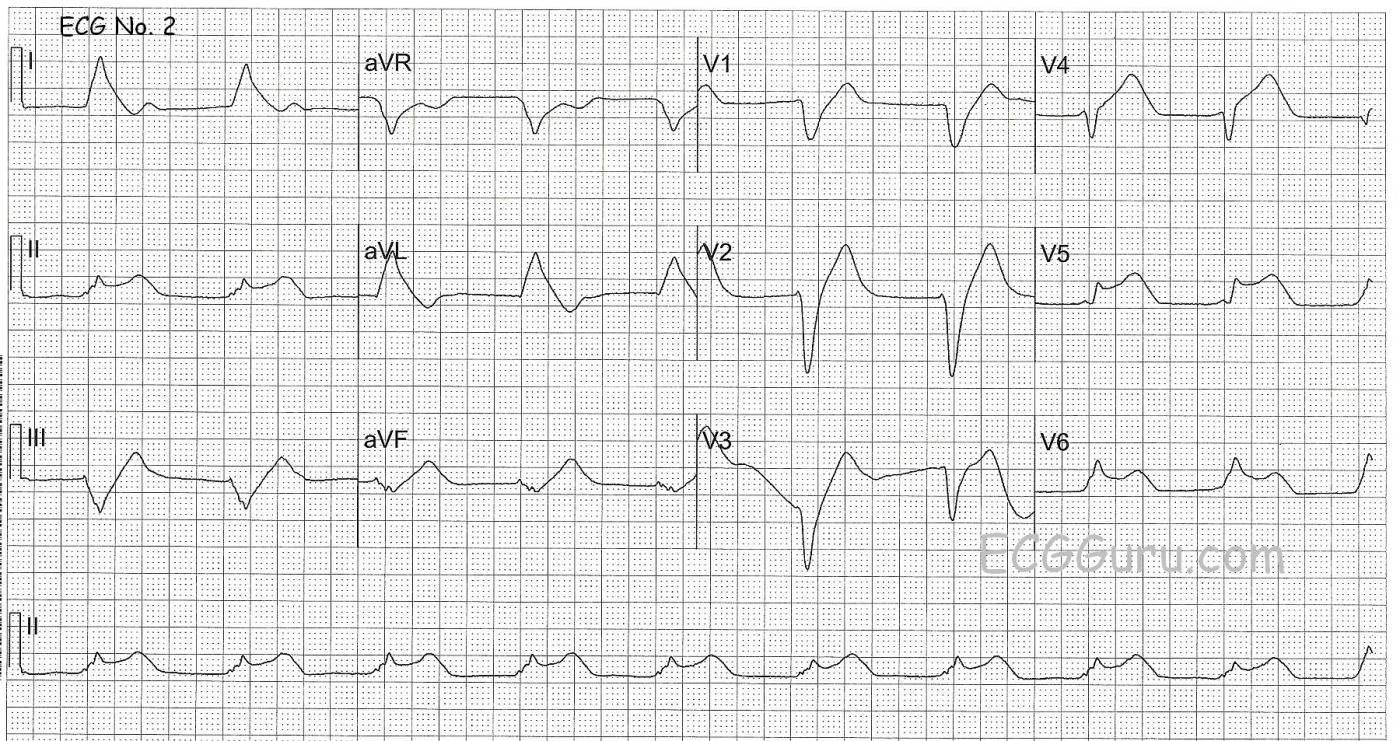
This series of two ECGs was obtained from a 41-year-old woman who was brought to the Emergency Department and subsequently suffered cardiac arrest. ECG no. 1 is pre-arrest and ECG no. 2 is post-arrest. We do not know the symptoms she presented to the ED with, or the type of arrest (bradycardic or VFib, for example). So, our discussion is speculative. But the difference between the pre- and post-arrest ECGs is striking.
Do you see any abnormalities in the first ECG which might indicate that an arrest is pending? Is there any clue to her medical problems? In ECG no. 2, do we see signs of the cause of the arrest, or are all the changes due to the loss of perfusion during resuscitation attempts?
Please join in the discussion in the comments below.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Why Did this Patient Arrest?
Interesting case, for which we unfortunately lack clinical information. ECG #1 (Pre-Arrest) shows sinus tachycardia at a rate just over 100/minute. There is low voltage, especially in the limb leads. The QRS is narrow. The principal abnormality is a prolonged QTc. This is subtle, and easy to overlook, because of the indistinctness of the end of the T way in many leads. That the QT is long is perhaps best appreciated in lead II, with confirmation that the QT makes up well over half the R-R interval. Considering the rapid rate (over 100/minute) — I’d estimate the QTc to be at least 480ms. Otherwise, ST-T wave changes are nonspecific. Common causes of a long QT interval include drugs — electrolyte disorders (low K+; low Mg++; low Ca++) — and/or CNS disorders — with need for correlation with the clinical history. Perhaps preexisting electrolyte disturbance (ie, hypokalemia) may have precipitated her arrest? Otherwise, although low voltage is clearly a nonspecific finding — knowing that this patient was about to arrest makes one wonder if entities such as pericardial effusion could possibly be relevant.
The Post-Arrest tracing ( = ECG #2) is equally interesting. The rhythm is fairly regular at ~60/minute; the QRS is wide; and P waves are lacking — defining this as AIVR ( = Accelerated IdioVentricular Rhythm). The dramatic terminal QRS widening present makes one wonder about a toxic effect, perhaps from poor perfusion during cardiopulmonary resuscitation. Despite presumed ventricular etiology for this rhythm — there appears to be primary ST elevation in at least leads II, V4,V5,V6. Whether this acute STEMI was the cause or result of the arrest may be impossible to tell without more clinical information ... — but regardless, the important clinical lesson to learn is that despite QRS widening and ventricuar etiology for the rhythm — there IS evidence of acute ST elevation on ECG #2 that indicates acute infarction. BOTTOM LINE: Even when key clinical information is lacking (as it sometimes will be in "real life" when patients are "found" ) — there are important clues that can be derived from careful scrutiny of available ECGs.
Ken Grauer, MD www.kg-ekgpress.com [email protected]