The Patient: This ECG was obtained from a man in his mid-sixties who was complaining of chest pain. The pain had an acute onset and is described as "10" on a 1-10 scale. He has a PMHx of coronary artery disease with stents in his right coronary artery and minimally invasive aortic valve replacement.
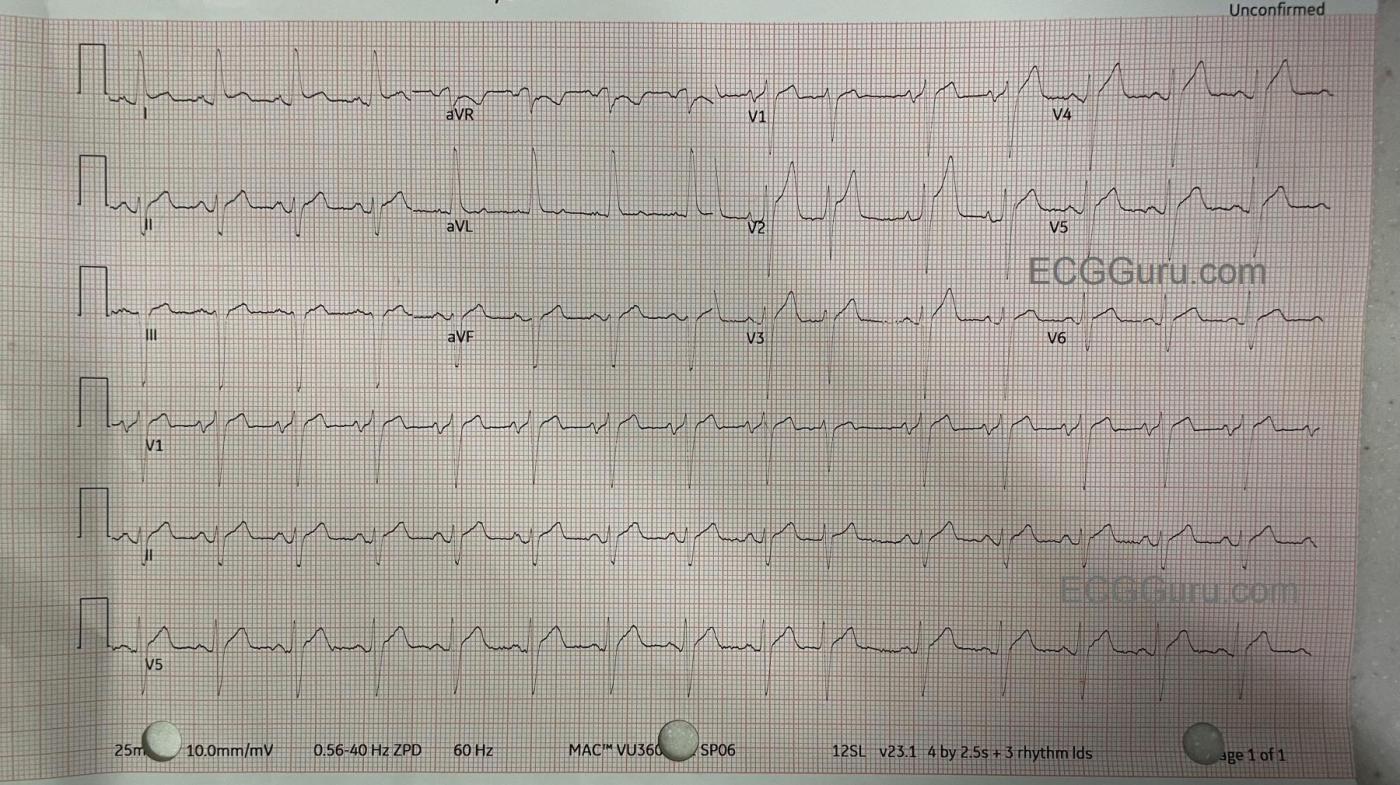
The ECG: The rate is 86 bpm. The rhythm is normal sinus rhythm with one PAC (10th beat). The PR interval is .18 seconds (176 ms), the QRS duration is .122 seconds (.12 seconds). This represents a ventricular conduction delay. There is no right or left bundle branch block. The QT/QTc is 333 ms/400 ms (B). The frontal plane QRS axis is leftward, with criteria for left anterior fascicular block. LAFB can be explained by this patient's history of prior CAD and valve replacement. There is ST elevation in Lead I and also in V1-V6. The ST segments have a straight shape in Leads I and aVL and in V1-V6. This shape represents ischemia in a patient with these symptoms and ECG findings. This is an ANTERIOR-LATERAL OCCLUSIVE M.I.
Followup: The patient was taken to the cath lab and had angioplasty of an occlusive mid-LAD (left anterior descending) lesion and a partially-occlusive mid-RCA lesion.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute Ant-Lat STEMI until Proven Otherwise
Today’s patient is a 60-something year old man with known coronary disease — who presents with new 10/10 CP (Chest Pain). Therefore, even BEFORE reviewing this patient’s ECG — statistical odds favor him having an acute OMI, potentially with diffuse ST-T wave abnormalities on his ECG (consistent with underlying multivessel disease).
I see essentially the same ECG findings as described above by Dawn. There is sinus rhythm with a PAC — LAHB — and abnormal ST-T wave abnormalities in virtually 12/12 leads.
The most remarkable lead is lead V2 — which despite modest S wave depth (~10-11 mm) — manifests 3-4 mm of J-point ST elevation. An interesting finding (of ? significance) — is that maximal J-point ST elevation is seen in the post-PAC QRS complex in this lead V2. Regardless of what this might mean — we KNOW that the ST-T wave in lead V2 is disproportionately ( abnormally) elevated in this patient with new, severe CP.
We see similar slight ST-T wave variability among the 4 QRS complexes in lead V1 — with the “bottom line” that the ST segment straightening, elevation and T wave peaking in lead V1 is also clearly abnormal.
ST-T wave findings in the remaining chest leads are a bit more subtle — but each of these remaining 4 chest leads manifest abnormal ST segment takeoff straightening with “too much” J-point ST elevation in leads V3,V4,V5.
In the limb leads — there is hyperacute ST elevation in lead I. Given the chest lead findings that suggest acute anterior MI — it is usually lead aVL much more so than lead I, that supports our supposition of acute anterior MI by finding ST elevation in lead aVL. However — there is no ST elevation in lead aVL in today’s ECG. Given the overall ECG picture that I have just described — I suspect this is the result of today’s patient’s longterm inferior wall injury (and partially-occlusive RCA lesion on today’s cath).
Otherwise — there are abnormally straightened ST segment takeoffs in each of the inferior leads — and an unusual (probably reciprocal) shape of ST coving, J-point depression and T wave inversion in lead aVR.
Bottom Line — Exactly as Dawn predicts — the above ECG findings in this patient with new, severe CP and known coronary disease — must be assumed to indicate acute LAD occlusion until proven otherwise. Timely cardiac cath confirmed this ECG impression.
Ken Grauer, MD www.kg-ekgpress.com [email protected]