The Patient: This ECG and rhythm strip are from a man in his early sixties. He was in his cardiologist’s office, complaining of a very rapid heart rate and weakness for several hours. He was standing, and denied pain, shortness of breath, or dizziness. The vital signs were not shared with us, but the patient was warm and dry, alert and oriented, and ambulatory. We are told that he has an unspecified myopathy and an automatic implanted cardioverter/defibrillator (AICD).
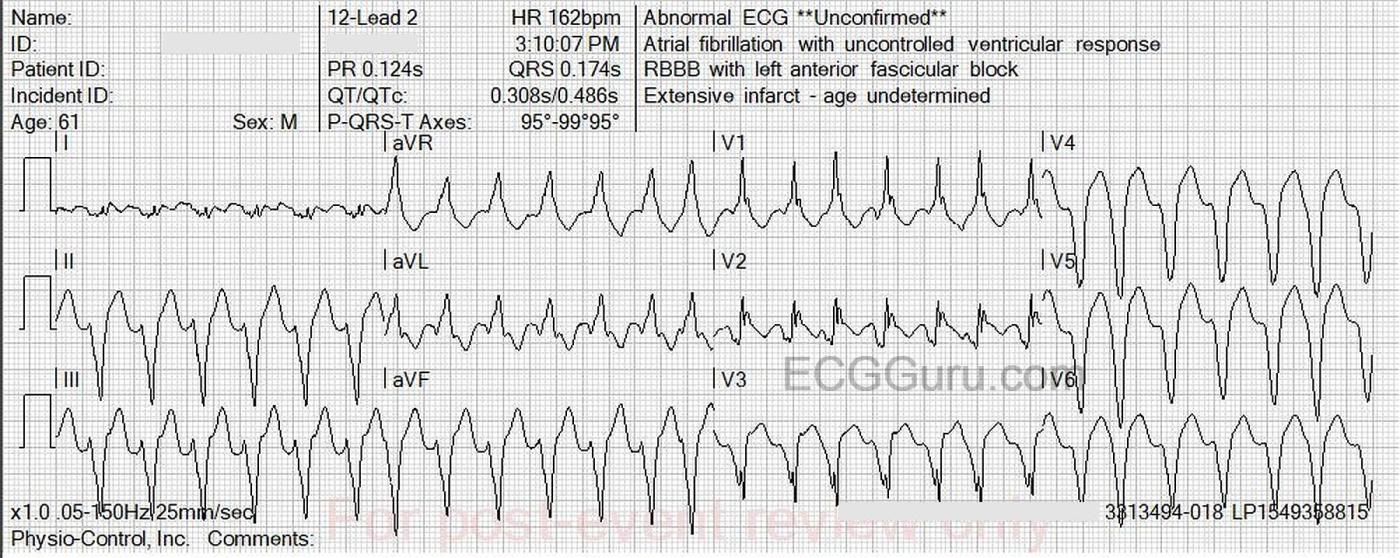
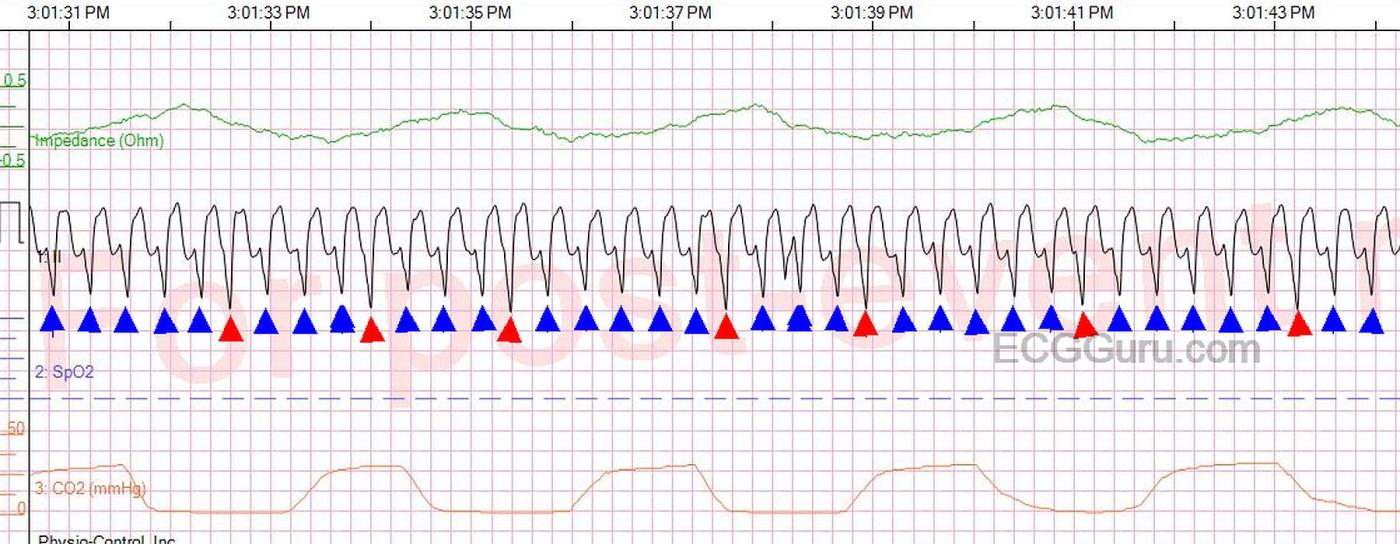
The 12-Lead ECG: There is a wide complex (0.174 sec.) tachycardia (WCT) at 162 bpm. The rhythm is slightly irregular, triggering an interpretation of “atrial fibrillation” by the machine. The computer also suggested right bundle branch block and anterior fascicular block (bifascicular block). I do not agree with this. I see a WCT that does not have the typical QRS pattern of RBBB or bifascicular block. There is an underlying REGULAR rhythm, with occasional premature beats that resemble, but are not identical to, the regular beats. (See rhythm strip included).
This rhythm is V Tach. Often, especially in an emergency setting, V Tach is a re-entrant tachycardia, characterized by a sudden onset and offset and a fast, regular rhythm. In this case, the V Tach is interrupted every 3-5 beats by a PVC. This tells us that the V Tach is due to increased automaticity or triggered activity, as a PVC would abolish the re-entry cycle. The PVCs look very similar to the “regular” V Tach beats, but are not exactly the same. So, the PVCs are coming from a focus very near the origin of the V Tach. This regular rhythm with frequent PVCs is easier to appreciate on the long rhythm strip provided, which rules out atrial fibrillation.
There are many different patterns associated with V Tach, with QRS morphology determined by the site of origin of the V Tach. The clinical implications and management vary by the origin of the V Tach. I highly recommend Dr. Jerry W. Jones’s book, “Getting Acquainted With Wide Complex Tachycardias: A Workbook for the Electrocardiographically Confused”. Dr. Jones covers V Tach and other WCTs in a very engaging workbook style. It is designed for healthcare professionals with intermediate ECG skills to improve their ability to diagnose and manage WCTs. Available wherever you get your books.
This V Tach has many characteristics of posterior fascicle or papillary muscle V Tach. If you want to dive into this topic (for intermediate to advanced ECG nerds), here are some links.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6434512/
https://litfl.com/idiopathic-fascicular-left-ventricular-tachycardia/
Patient Follow Up: The patient was given Amiodarone pre-hospital, and arrived in the Emergency Department in unchanged, stable condition. His AICD was interrogated, and he was determined to have monomorphic V Tach. He was cardioverted, and adjustments were made to the device. He had elevated troponins, attributed to demand ischemia. He was discharged home after two days, to resume medical management of the ischemic cardiomyopathy.
Our thanks to Jessica Banks, RN, EMT-P for donating this case.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Sustained VT with PVCs!
Today's case by Dawn is remarkable for the simultaneous presence of sustained VT with intermittent but persistent PVCs. I'd add the following points to Dawn's presentation.
The underlying rhythm in today's case is a regular WCT ( = Wide-Complex Tachycardia) at ~160/minute, without clear sign of atrial activity. Statistically — given this patient's older age and known heart disease — the likelihood that this rhythm is VT even BEFORE we look at the ECG is over 90%.
We can increase this statistical likelihood that the rhythm is VT to over 98% by considering: i) That this patient "has been there" — in that he already has an AICD; — and — ii) QRS morphology is all-but-diagnostic of VT, given complete negativity of the QRS not only in lead V6 — but also in leads V3,V4,V5. The remaining 2 chest leads also strongly indicate VT because of: iii) The lack of an S wave descending below the baseline in the all-positive QRS in lead V1 (that manifests a "taller left rabbit ear") — and — iv) The dramatically widened initial Q wave in lead V2 — that in my experience is a "tell-tale sign" of VT.
So — this patient has an AICD — but he presents in sustained VT. As a result — we need to assume malfunction of the AICD (which as per Dawn, was done in the hospital). Given this patient's underlying disease — a functioning AICD will be essential to this patient's longevity.
The simultaneous occurrence of sustained VT with frequent superimposed PVCs is not common. Today's case is insightful as to what this combination may look like.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Fascinating ECG! Thanks!!
Thanks for alerting me to this ECG!
It is indeed a monomorphic VT originating in the left apical area. And it is likely coming from the left apicolateral wall since precordial transition had occurred before V1. I think we can safely say that the mechanism of this VT is due to enhanced automaticity. If you note: when the PVCs appear, they always reset the automatic pacemaker and the R-R interval following each PVC is the same as the regular R-R intervals, indicating a pacemaker reset. This makes a papillary muscle VT much more likely. A reentrant VT would be terminated by the PVC and a VT due to triggered activity would also likely be terminated.
BTW, the CAPTCHA code I had to copy to insert this comment spelled out a really dirty word! ;-)
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd