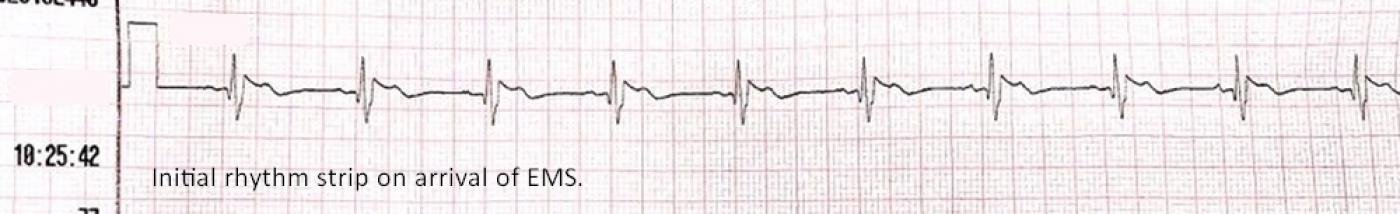
The Patient: This ECG is from a 59-year-old woman who was found by the EMS crew to be unresponsive, with agonal respirations at about 6 breaths per minute. Her pulse was thready at the carotid, and absent peripherally. Her skin was pale, cool, and mottled. Her BP via the monitor is 81/40, peripheral pulses not being palpable. An initial rhythm strip showed sinus rhythm at 75 bpm with right bundle branch block and ST elevation.
The patient’s husband gave a history of “difficulty breathing” since sometime this morning, alcohol dependence, hypertension, tobacco use, and insomnia. He said she had been drinking heavily for several weeks.
She was immediately ventilated and intubated, and an intraosseous infusion line established. A12-lead ECG was done, and it showed a dramatic change in the rhythm and ST segments over the initial strip. She was transported to a nearby hospital with CPR support. She achieved return of spontaneous circulation (ROSC) at the Emergency Department, after having three doses of epinephrine. Follow up with the ED physician revealed that the patient had suffered a massive gastrointestinal bleed. This patient, due to loss of a critical amount of blood, had low blood pressure and very poor perfusion, which resulted in damage to her heart (and possibly other organs as well). I do not have further follow up, but will update this if I receive more information.
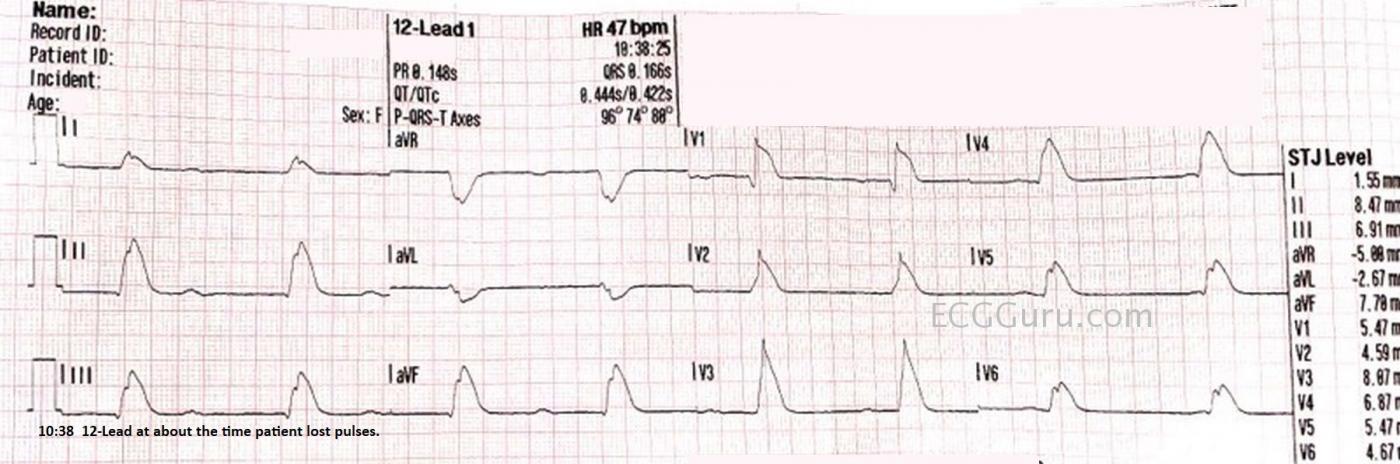
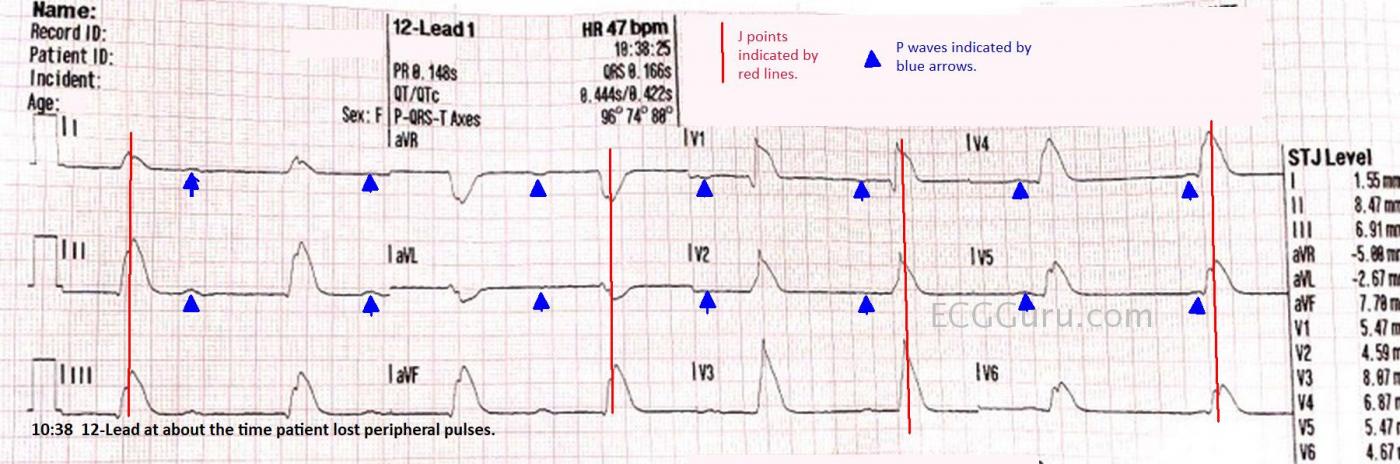
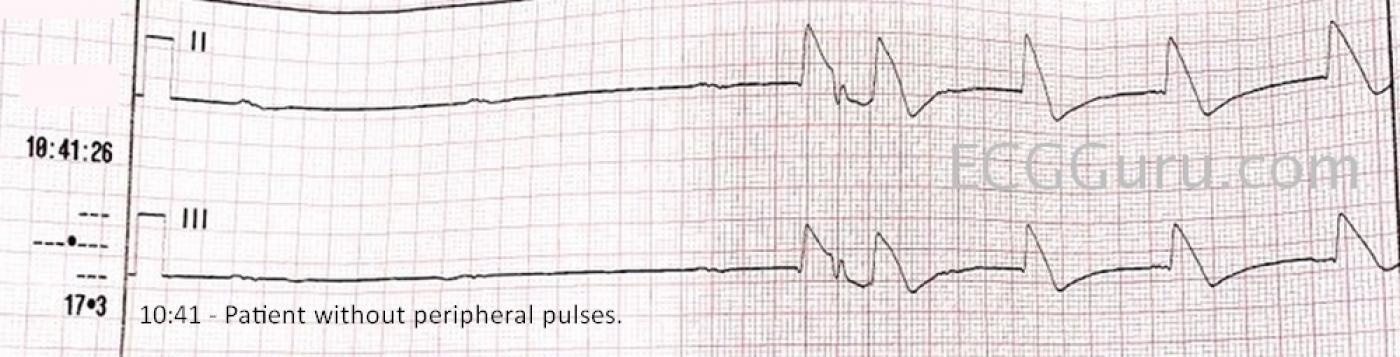
The ECG: The 12-Lead ECG done several minutes into the call is very different from the original rhythm strip. The P waves are slightly irregular, with an average rate of about 47 bpm. (Marked with blue arrows on the labeled ECG). The QRS complexes are also slightly irregular, but not at all related to the P waves. It appears to be a right bundle branch block pattern, with a pathological Q wave in V1. Because of the ST changes, it isn’t possible to discern a small S wave in Leads I and V6, as we would normally see in RBBB. This appears to be a junctional rhythm that averages about 51 bpm. I would call this a complete heart block, even though complete heart block usually implies that the atrial rate will be faster than the escape rhythm. In this ECG, I see no signs of the P waves conducting, even when they have ample opportunity – that is, they have not fallen into a refractory period. In fact, a few minutes after the 12-lead ECG was done, there was a period recorded of about four seconds with P waves only.
The most notable feature of this ECG is that there is extreme ST segment elevation in all leads except aVR and aVL. The J points are so high, it appears that the QRS complexes are extremely wide. A second view of this ECG is provided with the J points marked with red lines to help you see where the QRS ends and the ST segment begins. These types of ST segment elevations are often called “shark fin” pattern. Rather than wide QRS, this pattern represents a blending of the QRS and T wave. Shark fin pattern is often seen in “related leads”, leads that are oriented to one coronary artery. In this case, the ST elevations are very widespread. Without knowing this patient’s outcome, I can only make an educated guess, that this is a Type 2 M.I. Type 2 M.I. is defined as an M.I. caused by a mismatch between cardiac supply and demand, rather than by thrombosis. Especially in coronary arteries that are narrowed by disease, a low-perfusion state can cause myocardial damage and elevated troponins. This patient has severe hypovolemia and anemia due to her G.I. bleed. Another possibility is an occlusion from a thrombus in a dominant artery. For example, one of the branches of the left coronary artery could wrap around and perfuse the inferior wall, which is usually the right coronary artery's territory. An occlusion in a markedly dominant artery can cause widespread ST changes. I would be very interested in hearing your thoughts on this.
For more information on shark fin pattern, and myocardial infarction in general, we highly recommend Dr. Steven Smith’s excellent blog. Dr. Smith is an authority on M.I. ECG changes, and the shark fin pattern. http://www.hqmeded-ecg.blogspot.com
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
"Shark Fin" ST Elevation
Unfortunate case of this 59-year-old woman, who was found unresponsive with agonal respirations by EMS. The patient was markedly hypotensive with a massive GI bleed. Although definitive answers regarding this case are lacking — the initial 12-lead ECG is worth of mention.
• The cardiac rhythm appears to be complete (3rd-degree) AV block. Dawn has marked out fairly regular P waves (BLUE arrows). The QRS is wide and fairly regular, with continually changing PR interval. Given that P waves have more than adequate opportunity to conduct on this tracing — this qualifies as complete AV block.
• As per Dawn — the most remarkable feature of this ECG is the “shark fin” pattern of dramatically elevated ST segments in virtually all leads. Numerous cases of this phenomenon have been illustrated on Dr. Smith’s ECG Blog. I’ll refer you to the November 22, 2019 post, with my detailed Comment at the bottom of that page. I cite the informative quote by Dr. Pendell Meyers — “When the QRS is wide, the J-point will hide. So, your next move is to Trace it down, and Copy it over”. This was done in the tracing in this ECG Guru post by Dawn, in the form of vertical RED lines that indicate the J point in each of the 12-leads. So, the QRS complex is not as wide as one might initially think!
• “Shark Fin” ST segment elevation is commonly associated with acute LAD occlusion. That said — the history in this case is not one of chest pain — but rather severe blood loss from massive GI bleeding. This leaves me uncertain why instead of the usual picture of diffuse subendocardial ischemia (with diffuse ST depression + ST elevation in lead aVR) — we instead see diffuse ST elevation? Could there be coronary thrombosis instead of, or in addition to diffuse subendocardial ischemia from massive GI bleeding? Unfortunately, we lack the follow-up needed to answer this question.
• Additional ECG findings on this tracing include RBBB — a large Q wave in lead V1 (which in association with RBBB, usually means infarction) — small q waves in the inferior leads of uncertain significance — and reciprocal ST depression in lead aVL. We do not see a LAHB (or LPHB) pattern that most often accompanies Shark Fin ST elevation due to LAD occlusion.
BOTTOM Line: If you work in emergency care — you will on occasion encounter this Shark Fin pattern of dramatic ST elevation. Awareness of this pattern is essential — so that it is not misdiagnosed as a wide QRS without acute ST elevation (See this Dr. Smith post from June 11, 2018).
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Great Teaching Case!
This is an incredible teaching case and a rare but extremely important ECG pattern!
First, I want to reiterate and support a comment by both you (Dawn) and Ken: this is 3rd degree AV block because the P waves fail to conduct when they could reasonably be expected to conduct. It is NOT 3rd degree AV block because the P waves and QRS complexes are dissociated! I was recently shown some recommended study material for cardiology fellowship graduates to prepare for their boards. It made NO DISTINCTION between 3rd degree AV block and plain AV dissociation! These were CARDIOLOGY BOARDS! And if you surf the net a little bit, it won't be long before you encounter some websites that say the same thing. Marriott always hammered in the point that it wasn't AV dissociation that defined 3rd degree AV block - it was the failure of P waves to conduct when they should.
And Dawn, I agree totally that this is a Type 2 myocardial infarction - cath lab would be of no immediate help. I think this pattern is due to previously existent stenoses in the course of the LAD - probably supported by collaterals from the RCA and/or LCx. When the patient became shocky, the LAD lost that support and developed transmural ischemia in the LAD distribution. Hence, we have what appears to be an infarction involving the full extent of a Type 3 ("wrap-around") LAD.
There is a RBBB which is not unexpected with proximal involvement of the LAD. The qR morphology in V1 is a bit problematic. It frequently implies right ventricular strain and overload (which could be occurring here) but sometimes it may indicate the pathological q wave of infarction. Sometimes, however, it just indicates an rsR' morphology in which the r wave vector is perpendicular to Lead V1, making the s wave appear as a q wave.
I have no good explanation why the QRS in aVL is negative. With a proximal occlusion (or in this case, "involvement") of the LAD, one would expect STE in aVL that is partially or fully attenuated by the STE in Lead III. But, as Ken recently commented elsewhere, there's basically no accounting for anomalous anatomy or collateral circulation.
With this patient in shock due to GI bleeding (likely due to advanced cirrhosis and alcoholic gastritis and/or esophageal varices), clotting is not likely to be an issue here.
Thanks again for a remarkable case!
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd