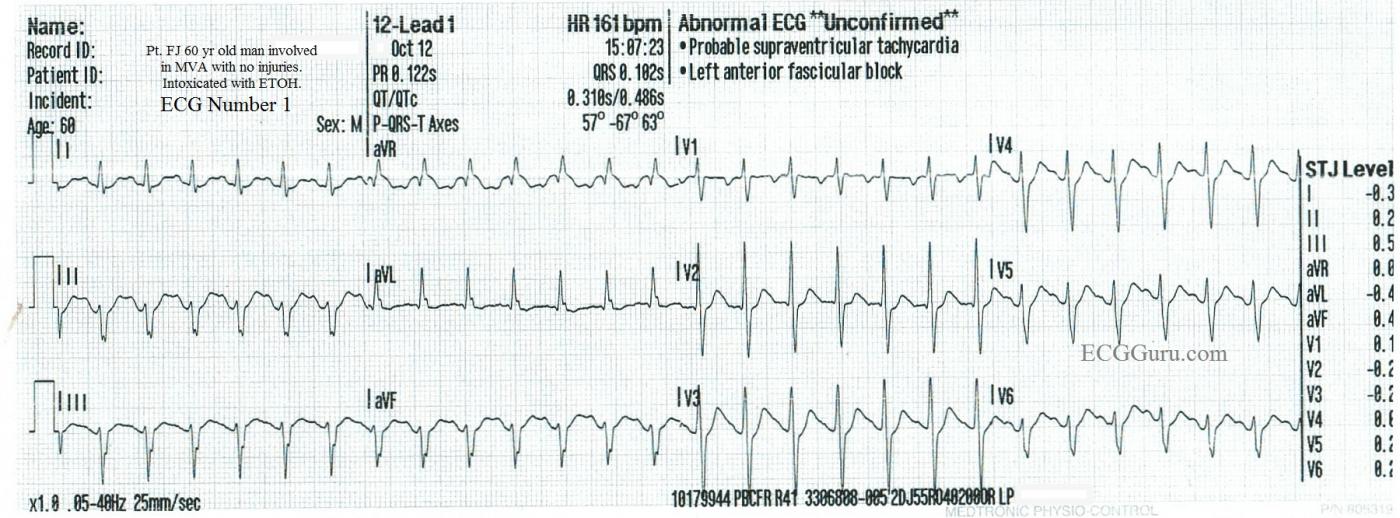
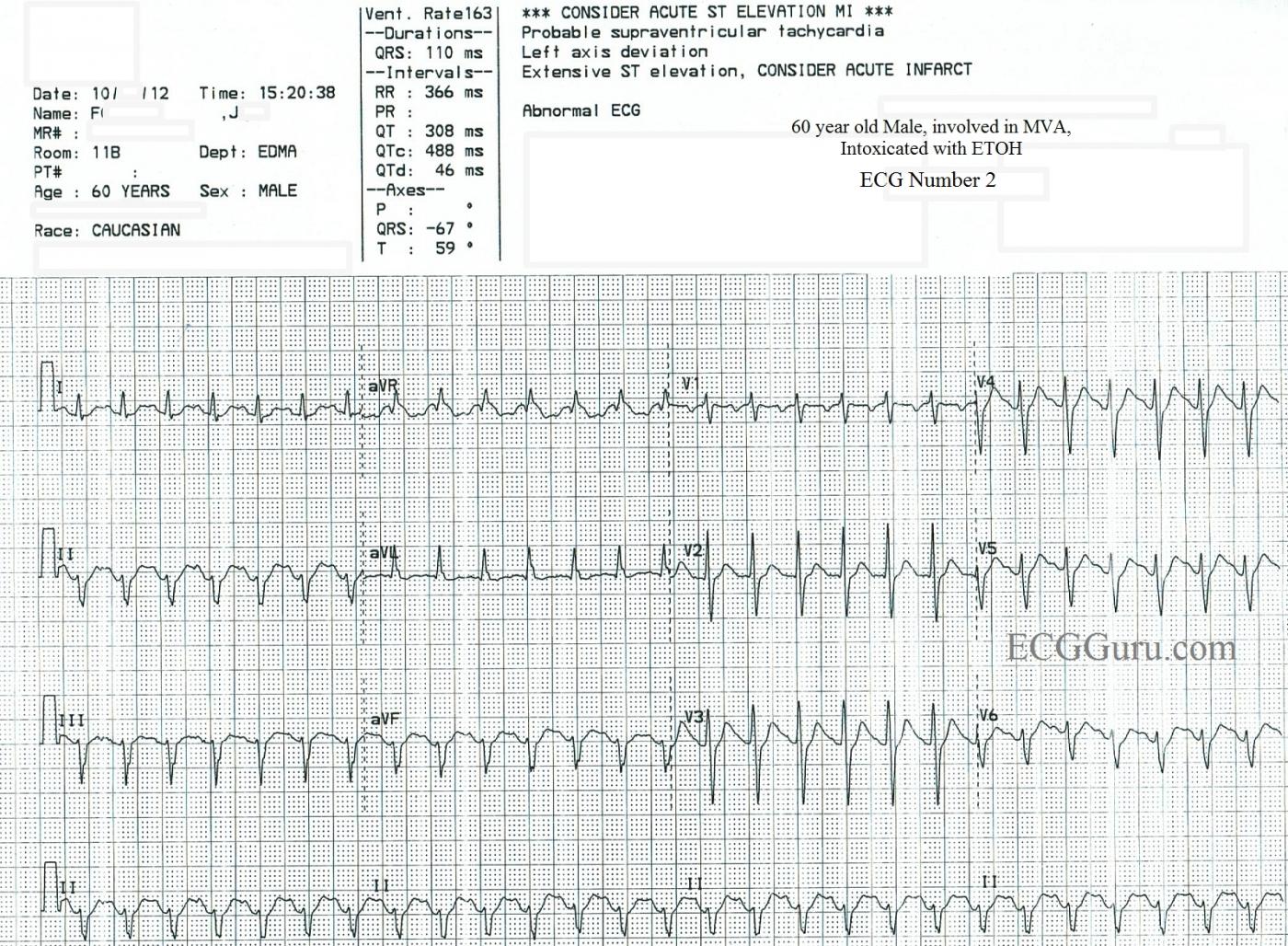
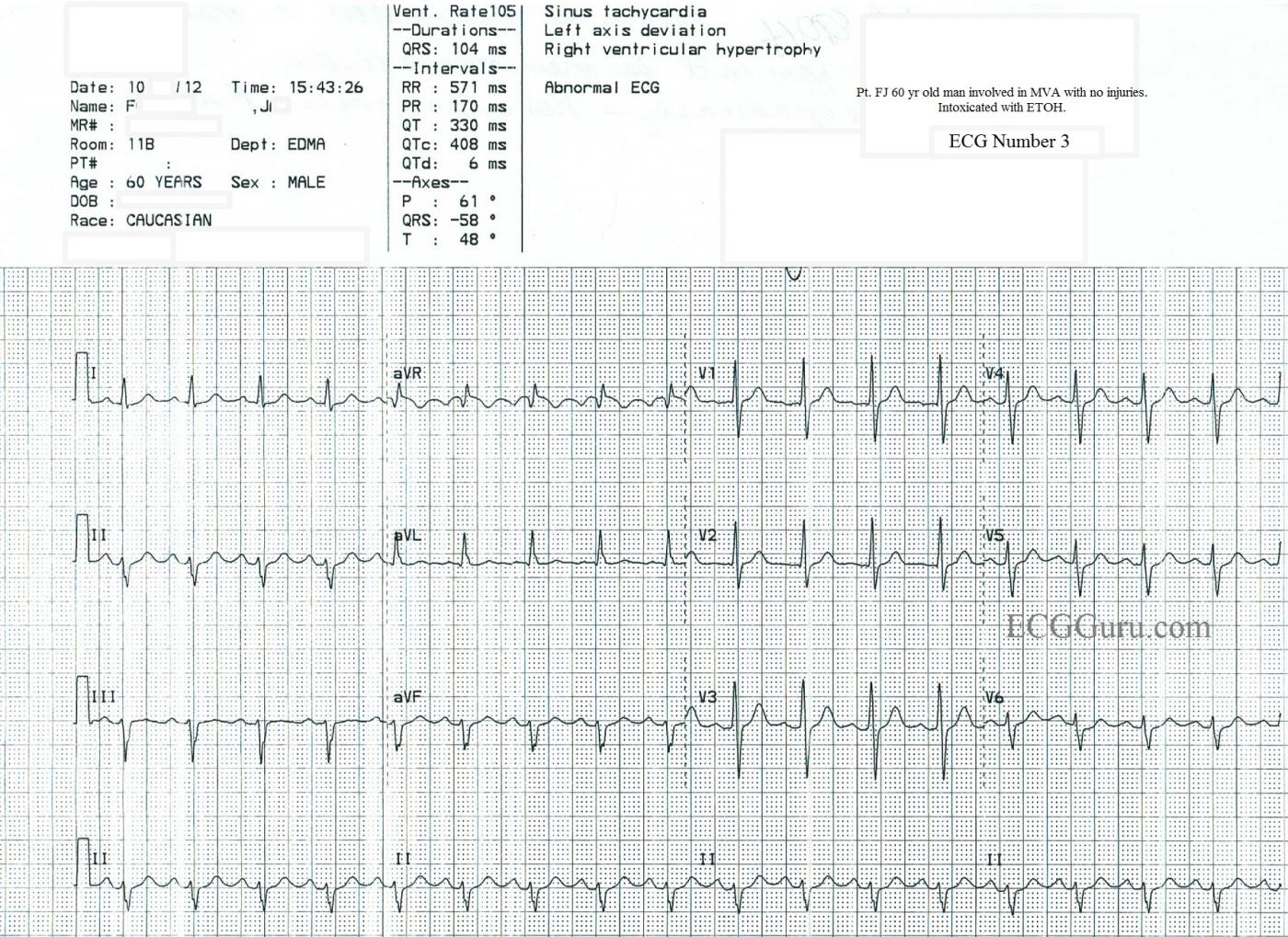
This series of ECGs was obtained from a 60-year-old man who was involved in a one-car accident. He sustained no injuries, but his blood alcohol level was far above the legal limit for intoxication at over 300 mmol/L. ECG No. 1 shows the ECG obtained by paramedics in the field, which they incorrectly interpreted to be atrial fibrillation. No medication was given. The ER physician obtained ECG No. 2, and considered sinus tachycardia as the diagnosis, but also, because of the fast rate and the fact that the rate had not changed for at least 15 minutes, he considered SVT or atrial flutter with 2:1 conduction. The ERP administered diltiazem (Cardizem) to the patient, which resulted in ECG No. 3. The transition to the slower rate was not captured on rhythm strips, but the nurse's notes showed a gradual change over 15 minutes from a rate of 160 to 105/min.
Usually, on the Instructors' Collection ECGs, we like to give the "answer". In this case, however, there will undoubtedly be some discussion regarding what went on. This discussion can be useful if you are teaching intermediate to advanced students. Questions to consider: 1) Is the fast rhythm an SVT and, if so, which one? 2) Is it sinus tachycardia and, if so, what are the effects of the car accident and the alcohol? 3) Is the left anterior fascicular block relevant? (Criteria are left axis deviation, slightly widened QRS complex at 110 ms, no other obvious reason for the axis deviation). 4) Is the ST elevation in the inferior wall during the tachycardia a sign of acute M.I.? The patient was lost to followup, so it is not known whether the ST changes were investigated. Note the flat ST segment and inverted T waves in V1 during the tachycardia that resolve when the rate decreases.
Please log in to register your comments on this interesting series.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Regular SVT - Sinus Tach vs Flutter vs PSVT?
Interesting series of tracings for which there are no defnitive answers (lost to follow-up) - so the "good news" being that NO ONE will be "wrong" with whatever hypothesis is proposed ...
RHYTHM First - The ED physician was right on target with his/her differential for a regular SVT in which one can't be certain about the presence/nature of P waves. 3 entities are by far the most common to consider. These include: i) Sinus Tach; ii) Atrial Flutter; and iii) PSVT. I'm actually surprised that choice for Diltiazem rather than Adenosine was made - since IF in fact this rhythm is Sinus Tach - then treatment is the treatment of the underlying disorder in almost all instances (on rare occasions beta-blockers in low dose might be contemplated to attenuate enhanced sympathetic tone). Assuming this patient was drunk but "stable" - there would not necessarily be need to slow him down unless the rhythm persisted ... That said - you CAN'T argue with success since the tachycardia resolved after the Dilt ...
Alternative options could have been:
I think this is probably all Sinus Tachycardia:
One often needs a "tincture of time" to "prove" sinus tachycardia. By that I mean - sinus P waves may be partially (or totally) hidden within preceding T waves - but with time (and correction of the underlying cause of sinus tach) this relationship changes. In support of this is the nurse's account that after Dilt the rate gradually changed over 15 minutes (whereas with PSVT there should be a much faster, abrupt change ....). The final result is sinus tach at 105/minute (which is what you expect for an inebriated patient).
I don't think the negative deflection in V1 during tachycardia was a "T wave" - but rather a P wave (the P wave of sinus tach). Granted - I no longer see this negative P in V1 after conversion to sinus rhythm (which actually is what bothers me most about my above hypothesis ... ) - but note the CHANGE in QRS morphology to a much taller R wave in V1 after conversion - so perhaps lead placement is different accounting for loss of the negative sinus P wave in V1 in this patient ....
As to the rest of the ECG - there is as mentioned LAHB - plus persistence of precordial S waves up to V6. One expects some ST depression during tachycardia - and although I do see some elevation of the ST segment in inferior leads during tachycardia - to me this looks more like a tachycardia T wave than stemi elevation. I see NO acute changes on the post conversion tracing - only the LAHB and the much taller R wave in V1.
The isolated finding of LAHB is of uncertain significance. If there is no underlying heart disease - there really are limited (if not no) prognostic implications. The Tall R in V1 should bring forth its own differential list - but given that the QRS is narrow, this is NOT wpw and not rbbb. It is not RVH - it could either indicate previous posterior MI or be a normal variant (perhaps due to body habitus given persistence of precordial S waves with low amplitude r waves in V5,V6).
FINAL THOUGHTS: Hindsight is 100% in the "retrospectoscope". I would have guessed sinus tach all along. I think I would not have treated so soon with Dilt, but would have worked on correctling other factors in this inebriated mva patient. My diagnosis might be confirmed if I saw gradual subtle (ie, from 160 to 158 to 156/min) reduction in heart rate over time (which is the best way to confirm suspected sinus tach). IF I felt "a need to know sooner" that this wasn't PSVT - adenosine could give a quick ED answer. And we'll never know for sure since the patient was lost to follow-up.
NICE CASE!
For anyone interested - this is the LINK to my ACLS Comments on the NARROW Tachycardia.
Ken Grauer, MD www.kg-ekgpress.com [email protected]