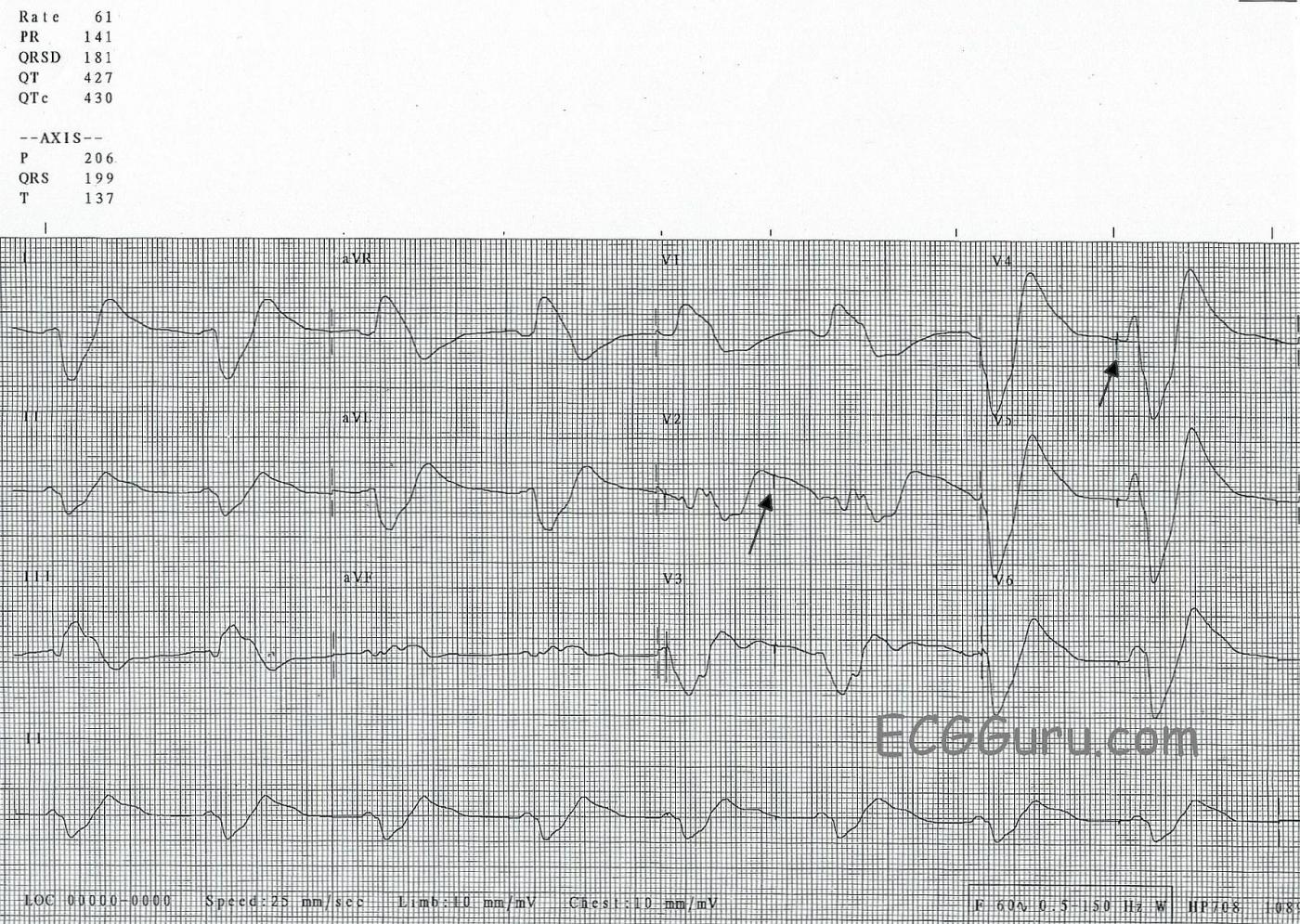
This ECG was taken from an elderly man who was in acute renal failure, and had presented to the Emergency Department via EMS. He was weak and hypotensive. We have no other medical history or clinical information.
The most noticeable feature of this ECG is the wide QRS, which is difficult to measure because there is no distinct J point at the end of the QRS complex. As a result, the QRS blends into the ST segment and T wave. The T waves are extremely wide. At a rate of 61 bpm, it is almost bradycardic. It appears that P waves may be present in some leads (like Lead II) - but, if so, the PR interval looks short. It is difficult to tell where the P wave ends and the QRS begins. Also, there are occasional pacer spikes, which are not capturing.
This is the “sine wave” rhythm of extreme hyperkalemia. This pattern usually appears when the serum potassium levels are well over 8.0 mEq/L. Had we seen the earlier ECGs, we might have had more warning, because the ECG in earlier stages of hyperkalemia shows us distinctive peaked, sharp T waves and a progressive intraventricular conduction delay (IVCD). See example. The intervals progressively widen, the P waves lose amplitude until they disappear altogether. It is as if someone is holding the tracing at each end, and stretching it apart.
At this stage, this is an immediately life-threatening condition, but usually treatable. Quick action must be taken to prevent cardiac arrest.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
The Cause of Extreme QRS Widening
This week’s ECG illustrates the phenomenon of extreme QRS widening. One might be tempted to diagnose acute infarction from the apparent ST elevation in leads III and aVF of this tracing. Instead, I think of the following considerations:
#1 — Is the patient hemodynamically stable at the time this tracing was recorded? Although weak and hypotensive — this patient was not pulseless and unresponsive. Therefore, this exceeding wide and formless set of complexes does not represent an agonal rhythm …
#2 — What is the paper speed? One gets accustomed to the paper speed most commonly used in the area where one resides. In the United States, this is most commonly a paper speed of 25 mm/second — but not necessarily so for other parts of the world (some of which routinely use 50 mm/second). The effect of using a paper speed of 50 mm/second (which is twice as fast as the 25 mm/second that I am accustomed to seeing) is to seemingly slow the rate (because the R-R interval doubles) and to widen the QRS to twice the width it would be if the paper speed was 25 mm/second. That said, we can see at the very bottom of this tracing that paper speed was 25 mm/second — so the slow rate and exceedingly wide QRS is accurately portrayed on this tracing.
#3 — What is the history? Exceedingly wide and amorphous QRS complexes as seen here should suggest either marked hyperkalemia or a severe toxic/metabolic disorder. The history of acute renal failure strongly favors the former. So does the fact that the patient was still alert with a recordable blood pressure, as consciousness would almost invariably be lost with overdose or other metabolic entities by the time QRS widening to the extent seen here had taken place. Given this history, severe hyperkalemia should be presumed even before the serum potassium level returns — and, empiric IV Calcium is immediately indicated. The onset of action of IV Calcium for emergency treatment of severe hyperkalemia is within minutes. The QRS complex should quickly begin to narrow, tall peaked T waves will return, the heart rate should increase, and atrial activity should become more evident.
Bottom Line: While the ECG picture of mild-to-moderate hyperkalemia is a far more familiar sight to many clinicians (with tall, peaked T waves; loss of P waves; moderate QRS widening) — one should not forget the picture of pre-lethal hyperkalemia, in which discrete QRS complexes and T wave peaking may be lost in the amorphous blend shown in this Figure.
--------------------------------------------------
Please NOTE these additional links for review of the ECG changes of hyperkalemia — and, the diagnostic dilemma of QRS widening.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Wide QRS in a Patient with Acute Renal Failure
Dawn...
A very challenging case indeed!
Even though this is an ECG interpretation site, I must say I was very impressed with Dr. Grauer's first statement which referred to the patient's clinical condition. And that's where I would start also.
Even as the techs are preparing to run a 12-lead ECG and the nurses are preparing the treatment for a presumed hyperkalemia, we must remember one thing - the term acute renal failure is somewhat of a misnomer. One is never suddenly stricken with renal failure as they might be with an acute MI, a stroke or a seizure. No one is ever feeling great and then suddenly collapses with acute renal failure. The acute renal failure is really a process that has been on-going for hours to days (instead of months to years - hence the use of the term acute). Most likely this patient has suffered some illness or condition that either resulted in prolonged hypotension or severe dehydration or loss of circulation to the kidneys (or all of that!). This did not happen just before the EMS arrived. Metabolic acidosis can also present a similar picture, although hyperkalemia is usually accompanied by a metabolic acidosis unless it is due to an over-ingestion.
Although this man needs stat empiric therapy (i.e., IV calcium) for hyperkalemia - NOT after waiting for a serum potassium level - I wouldn't be surprised if I gave the calcium and still saw a lot of problems on the ECG. The calcium followed by more potassium-lowering measures, however, would probably be life-saving.
I would also mention four caveats:
First, I would not place any faith in the association of specific potassium levels with findings on the ECG. To begin with, if I truly felt that I was dealing with hyperkalemia, I would not at all be concerned with any presumed level of potassium based on my ECG interpretation. Why? Because the earliest ECG findings of hyperkalemia - tall, peaked T waves - have on many occasions been the only finding at the time of cardiac arrest. I am always afraid that a new physician or other heathcare provider without a lot of experience treating patients with hyperkalemia will refer to one of those numerous "charts" relating potassium level to ECG findings and somehow think that that "Well, this potassium level is probably only 6.5 or so, therefore I have time to do a full work-up." People have been known to arrest with nothing more than tall, peaked T waves. I recently read a paper in which the authors stated that they would never give calcium for tall, peaked T waves because it just wasn't justified for "potassium levels that low." If the patient were a chronic renal failure patient on dialysis, I might agree. But even those patients can have very high potassiums levels before anything shows up on the ECG. Getting back to my original statement, I would not be concerned with the presumed level of potassium because any ECG changes suggestive of potassium elevation is still potentially lethal hyperkalemia!
Second, hyperkalemic T waves do NOT have to be tall nor come to a sharp point. However, they are typically symmetrical and often become very narrow just 1 or 2 mm above the baseline. They aren't always tall, either. So many novice ECG interpreters have difficulty distinguishing between the hyperACUTE T waves of an acute MI and hyperKALEMIC T waves. In their defense, there can be occasions when it really is difficult to tell which is which - even when you know the history (diabetic, on peritoneal dialysis with acute onset of ACS-compatible chest pain). The secret in most cases is to look at the T wave about two mm above the baseline. If the T wave suddenly narrows, that would be more typical (though not absolutely diagnostic) of a hyperkalemic T wave.
Third, hyperkalemic T waves are not always present. In fact, they are present only about 29% of the time according to one review paper. Although it's always important to know the other signs of hyperkalemia, it's even more important to know the patient's history so that you could reasonably suspect hyperkalemia even when the ECG signs are not so accommodating. (I say this because at this time much less emphasis is being placed on patient history and physical examination and more emphasis on prepared history templates and ordering tests before a patient is even seen.)
Fourth, when you give calcium you are not treating hyperkalemia! You are treating the effect of hyperkalemia on the relationship between the resting membrane potential and the threshold potential. Calcium will have absolutely zero effect on the serum potassium. So calcium must be given concurrently with other measures that can move the potassium inside the cell and/or eliminate it from the body.
The QRS complexes on this ECG are wide because the rising extracellular potassium has decreased the difference between the number of potassium ions inside and outside the cell. Thus, the resting membrane potential (RMP) is reduced, meaning it is not as negatively charged as before. It has moved closer to 0 potential. It is no longer as polarized as it was before the onset of the hyperkalemia and has therefore been partially depolarized. As the resting membrane potential becomes less and less negative, fewer and fewer sodium channels become available to open when a depolarization impulse stimulates the cell. As a cell is depolarized with fewer and fewer sodium channels available, the impulse (Phase 0) becomes weaker and weaker. This is manifested by a Phase 0 that has less amplitude and less slope (it loses its height and it leans more and more to the right). This is manifested on the ECG by a QRS complex that becomes wider and wider and less well-formed.
What does calcium do for all this? As the resting membrane potential becomes less and less negative due to the rising extracellular potassium level, it moves closer and closer to the normal threshold potential. In the beginning, this can mean that the heart rhythm can become very unstable because it takes less voltage to move from the RMP to the threshold potential. But it isn't long before the reduced difference in voltage has another effect - in moving from the reduced resting membrane potential to the regular threshold potential, there aren't enough sodium channels available to open to provide an effective depolarization, or Phase 0. Phase 0 is now losing its amplitude and sloping further to the right. It was discovered many years ago that adding calcium ions to the extracellular fluid moved the threshold potential closer to zero, making it also less negative. In moving it further away from the already partially depolarized resting membrane potential, more sodium channels become available to open, thus strengthening Phase 0 and returning its amplitude and slope closer to normal and making the QRS complex once again narrow and more normal-appearing. So we have made the QRS look much better and the resulting heartbeat much more stable and effective - but we still have the same potassium level! Don't forget the other potassium-lowering measures.
Getting back to this ECG, we learn that a prominent terminal R wave in Lead aVR is indicative of a tricyclic overdose. Be aware that some of these "findings" are actually based as much on the patient's history as on any physiological principles. It is the sodium-channel blocking capacity of the tricyclic antidepressants that cause the terminal R wave in aVR - just as it does in this patient with marked hyperkalemia and a patient with a toxic level of a sodium channel blocker! But, as Dr. Grauer alluded, a patient with a tricyclic overdose and an ECG that looks like this is typically unconcious with an impending seizure and/or cardiac arrest.
As for the lines that suggest the presence of a pacemaker - I'm not totally convinced that we aren't seeing artifact, but a pacemaker is certainly a possibility. While hyperkalemia and other metabolic disturbances can certainly interfere with capture, they should have no effect on sensing. The "spikes" occur only twice although they do appear in more than one lead. Pacemaker spikes are not hidden by the various deflections on an ECG - they can appear within QRS complexes, P waves and T waves. But here it looks like the pacemaker fired just twice during the whole strip. If this does not represent artifact, then one would have to assume a faulty pacemaker (possible, but statistically unlikely), over-sensing or the placement of a temporary VOO or transcutaneous pacemaker as the cause. Personally, from my own practical experience, I don't think most physicians would be fiddling with a pacemaker during the 10 seconds it takes to get the ECG upon which the patient's diagnosis and treatment may depend.
Hope this helps. Thanks for such an educational site!
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Thank you, Drs. Grauer and Jones
thank you both so much for taking so much of your time to write these instructive comments. I am so proud to be able to offer this kind of education to health care professionals I'm this website. I hope many of them are lucky enough to take your classes in person. I also hope people will feel comfortable to post QUESTIONS in this comment area, as it is amazing to have access to such knowledgeable instructors. Thanks again!!
Dawn Altman, Admin