A paramedic crew responded to the office of a local physician. A 61-year-old male presented with a one-week history of chest pain and shortness of breath. He had a previously undiagnosed atrial fibrillation with rapid ventricular response and left bundle branch block, but was alert. Shortly after transport commenced, the patient became unresponsive with Torsades de Pointes, which rapidly degenerated into ventricular fibrillation. The paramedic placed pads and defibrillated within one minute. After two minutes of compressions, the patient had a fairly regular rhythm with return of spontaneous circulation. Transport time was short. On catheterization, the patient was found to have severe coronary artery disease, requiring coronary artery bypass graft surgery (CABG) A balloon pump was inserted in an attempt to strengthen him for surgery.
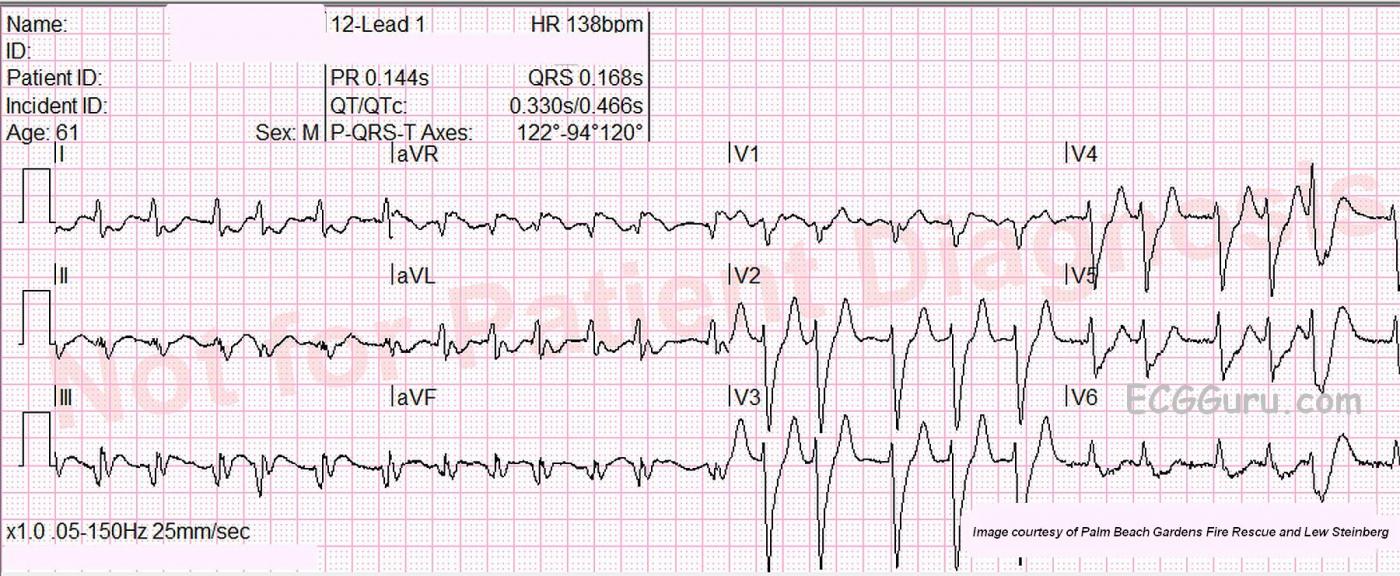
What is the rhythm? The 12-lead ECG presented here shows atrial fibrillation at a rate of 138 per minute. The rhythm is irregularly-irregular with no P waves. Since the patient had not yet been diagnosed with atrial fib, obviously no therapy had been initiated to control the rate. There is a PVC near the end of the strip.
Why is the QRS complex wide? The QRS complex is wide at 0.168 sec (168 ms). It meets the ECG criteria for left bundle branch block (wide QRS, supraventricular rhythm, negative V1 and positive Leads I and V6). Atrial fibrillation can lower cardiac output because there is no P wave, and therefore, no “atrial kick”. Left BBB can lower cardiac output because a wide QRS is a sign of unsynchronized depolarization of the ventricular muscle, which causes less pumping force. To help you determine if a rhythm is LBBB or VT, review Brugada's Criterion.
Are there ST changes? In wide-complex rhythms, it can be difficult to determine whether acute M.I. is present, because the wide QRS is normally accompanied by “discordant ST changes”. That is, if the QRS is positive, the ST and T wave are negative. If the QRS is negative, the ST and T will be elevated. In this ECG, there is a subtle ST elevation in Leads III and aVR, and subtle ST depression in I and aVL. It is difficult to attribute this to A.M.I., but subsequent events point to that as the diagnosis.
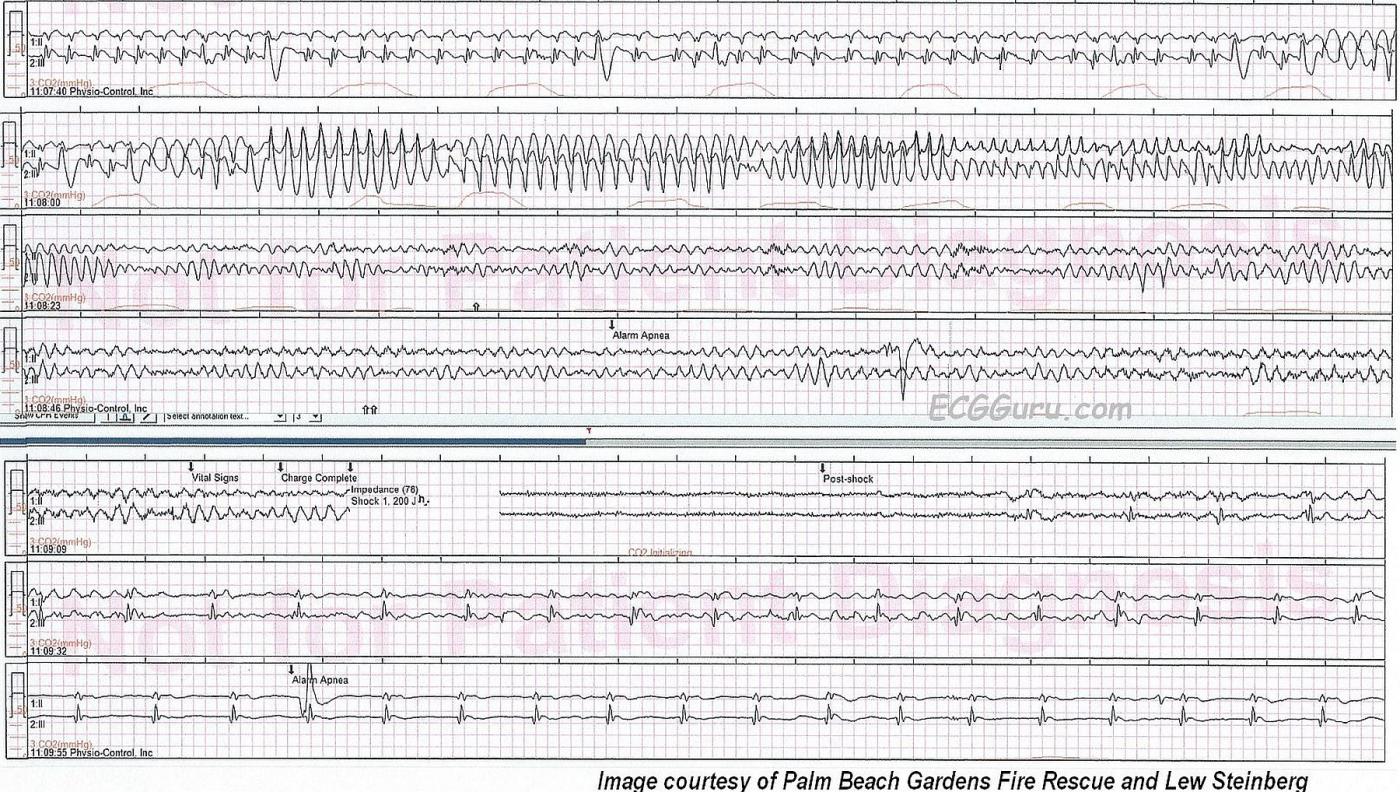
What about the rhythm strips that follow? The rhythm strips provided show the patient’s quick progression, during transport to the hospital, from atrial fib with PVCs to Torsades de Pointes, to V Fib. They show an electrical shock at 200 joules approximately 1 minute after the VT started. This shock successfully converted the patient’s rhythm. First, it appears that the rhythm may be atrial flutter with 4:1 conduction (or it may be baseline artifact). By the final strip shown, we see a regular rhythm without clear P waves at a rate of 50 bpm. This could be a junctional rhythm, difficult to assess with only a 2-lead rhythm strip.
This series provides many teaching opportunities.
1) Both atrial fib with LBBB and VT can cause a WIDE-COMPLEX TACHYCARDIA.
2) It can be difficult to see the classic signs of STEMI when BBB is present.
3) VT can progress VERY RAPIDLY to V Fib, especially in low-output conditions.
4) Effective chest compressions and quick defibrillation will often result in conversion to an organized rhythm. Defibrillating the perfused heart is infinitely more effective that shocking a poorly-perfused heart. Kudos to this crew for a job well done.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
IVCD, ST Changes, Torsades and More!
Our thanks to Lew Steinberg and Palm Beach Gardens Fire Rescue for submitting this high-quality 12-lead and cardiac arrest series. One could easily present a several-hour didactic session just using this case and these tracings! Having a positive response to resuscitation is an added benefit to this teaching case, with credit to the crew for a job well done!
The 12-Lead ECG — I believe the patient was still alert and perfusing at the time this tracing was obtained … which allows us a moment to contemplate the rhythm. As per Dawn, the QRS complex is clearly widened. No P waves are present. The rhythm is irregularly irregular. So even though we have a WCT ( = Wide-Complex Tachycardia) — this clearly looks like a supraventricular rhythm ( = AFib with rapid ventricular response) and not VT. Although VT may at times be somewhat irregular — it is rare to manifest the irregular irregularity that we see throughout the entire rhythm strip here.
QRS morphology is very unusual. I would not classify this as a LBBB because: i) despite negativity of the QRS in lead V1, we see a notched small S wave rather than a definite and deeper QS complex; ii) substantial r waves already develop by V2 (whereas r waves are generally smaller in these leads with LBBB); iii) we lack a wide monophasic R wave in V6 (instead only seeing a slender tiny R wave); and iv) rather than a wide monophasic R wave in the lateral limb leads ( = I, aVL) — we instead have a multiphasic complex with considerable S waves. I therefore think the best classification of the conduction defect we see is IVCD (IntraVentricular Conduction Defect) — rather than LBBB.
Note the deep and wide Q waves in leads III and aVF. Although it clearly is more difficult to assess the significance of Q waves in the presence of a conduction defect — the appearance of these Q waves should strongly suggest infarction of uncertain age. In addition, there is much fragmentation of the QRS complex in a number of leads (perhaps most noted in lead II ) — which strongly suggests “scar” from cardiomyopathy and/or infarction of uncertain age.
Finally — there is a lot of ST segment deviation that just should not be there with this type of conduction defect. Specifically — there is ST-T wave depression in leads I, aVL, V5, V6 and probably also V4. ST segments are elevated in leads III and aVR. So despite the conduction defect — the “theme” to me is that of significant ST depression in multiple leads with ST elevation in leads III and aVR. Whether this is due to tachycardia, ischemia, infarction, etc. isn’t readily apparent from this single tracing — but these possibilities need to be considered. Last — the significantly peaked T waves in V2,V3,V4 are especially difficult to assess in the setting of marked tachycardia and IVCD. These may simply be secondary repolarization changes due to the conduction defect, and/or they may be due to the tachycardia. Alternatively — they might also reflect a De-Winter-like T wave abnormality from ongoing LAD occlusion … There just is no way to tell from this single tracing.
There are numerous teachable moments in the Cardiac Arrest Sequence that follows. It is hard to imagine a more typical Torsades de Pointes example than the one we see on the 2nd line of this sequence. One can quibble as to whether this is PMVT ( = PolyMorphic VT) vs true Torsades de Pointes, with distinction made because the QT is normal in the former and prolonged with Torsades. I strongly favor the latter, because despite the tachycardia — the QT interval in the leads such as V2, V3 on the 12-lead tracing clearly looks to be well over half the R-R interval.
Torsades then deteriorates to VFib, which is appropriately defibrillated. That this results in conversion to a supraventricular rhythm should be evident because of identical QRS morphology (at least in the bottom monitoring lead) as was seen during the initial AFib rhythm. I think the bottom 2 lines both reflect the same junctional escape rhythm at ~ 50/minute, with the baseline irregularities initially (in the 6th line) due to artifact that in large part resolves by the last line of this sequence. THANKS again to Lew Steinberg and Palm Beach Gardens Fire Rescue for sharing this highly insightful case with us!
-----------------------------
Additional Reading:
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Kudos to the Palm Beach Gardens Fire Rescue! A Job Well Done!
Dawn...
Thanks for one of the most interesting resuscitation scenarios I've seen in a while! But let's cut to the chase...
1. Untreated atrial fibrillation - Untreated atrial fibrillation typically has a ventricular rate > 120/minute, as does this patient.
2. I suspect (and I emphasize "suspect") there was an acute or (more likely) sub-acute inferior MI involved here - ST depression and T wave inversion in I and aVL and V5 and V6 with what I suspect would be STE in the inferior leads if the tracing were just a bit more stable (and perhaps done a day earlier). But there is also STE in aVR which would be more associated with a proximal LAD lesion. The ST depression in V5 and V6 also indicate LAD involvement. Furthermore, this patient had a CABG - not a PTCA with stent - and had to have a balloon pump for support. Neither of those is treatment for any type of dysrhythmia or typically for a single lesion in the LAD or RCA. Here is what I suspect happened - a day or two earlier, the patient probably suffered an occlusion of the RCA which wiped out the SA node resulting in atrial fibrillation. Atrial fibrillation in the setting of an acute MI is much more lethal than ventricular fibrillation under the same circumstances because the V fib is usually due to temporary myocardial irritability which will resolve while the a fib is due to a very destructive loss of myocardium. The RCA was probably shunting blood into an already heavily diseased LAD. The loss of this collateral circulation resulted in the STE in aVR and the ST depressions in V2 - V6. I'm not really sure what V1 is doing, but I suspect there was a bit of STE there at some point. Whenever you have an inferior MI along with ST depression in V5 and V6, you usually also have a very compromised LAD that was depending on collateral circulation from the RCA, and I suspect that is what happened here and why the patient received a CABG and not just a PTCA with stent.
3. One of the first things that caught my eye in the 12-lead were the sizable S waves in Leads I, aVL and V5. That isn't going to happen with LBBB - ever! Also if you look closely, you can see tiny septal q's in I and aVL and septal r's in V1. While you CAN have septal q's in aVL during LBBB and even a tiny r in V1 during LBBB that is due to a proximity effect (and NOT L to R septal conduction), a septal q in Lead I just isn't going to happen.
4. There is also a profound left axis deviation which could be due to inferior MI and/or LAFB. I suspect LAFB is at least involved because the peak of the R wave in aVL comes just before the peak of the R wave in aVR indicating a counterclockwise rotation favoring LAFB.
5. There IS a variant of RBBB that consists of an Rs in Lead I and an rs in V1 (no R' - just a small s). I can't say if that is what is occurring here, so I would agree with Dr. Grauer that it would be best to call this an IVCD.
6. With a rapid and fairly irregular rate, I'm not sure that I would be able to distinguish between Torsade de Pointes versus polymorphic ventricular tachycardia. TdP usually occurs in the setting of hypokalemia and a slow heart rate. We have no idea what this patient's K+ level was, but the heart rate certainly wasn't slow. PMVT usually occurs in the setting of high catecholamine levels and one could only assume that a patient in this much distress was probably experiencing that. We get a little preview of what's about to happen from the last beat in the 12-lead in which a PVC lands on a T wave.
7. This man would NOT have survived had it not been for the quick intervention by the Palm Beach Gardens Fire Rescue.
I wonder what this man's P waves would have looked like had he not been in atrial fib. I sort of get the impression that he might have been a heavy smoker.
Thanks, Dawn, for a really great teaching opportunity. And thank you, Dr. Grauer, for your insight. It looks like we were thinking along the same lines.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd