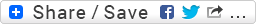
I performed this 12-lead ECG (Fig. 1) several years ago in the medical intensive care unit (MICU) while standing at the patient's bedside. As I was recording the ECG, I distinctly remember thinking to myself: "this patient looks REALLY sick!" for being as relatively young as he was. Immediately after I printed out the hardcopy, I reviewed the computer's interpretive statements at the top of the page. The computer listed an uncommon pair of findings which I confirmed to be true. I asked the assigned nurse if her patient had the clinical condition that this combination is highly suggestive of. She shrugged her shoulders at me and said she didn't know. I consulted the patient's computerized record and right there listed at the top of their "active problems" was the very condition I suspected the patient of having.
Patient's clinical data: 49-year-old black man with history of Type II diabetes mellitus (DM) and this other clinical condition.
Fig. 1: I performed this ECG exactly 5 months and 5 days before the ECG in Fig. 2.
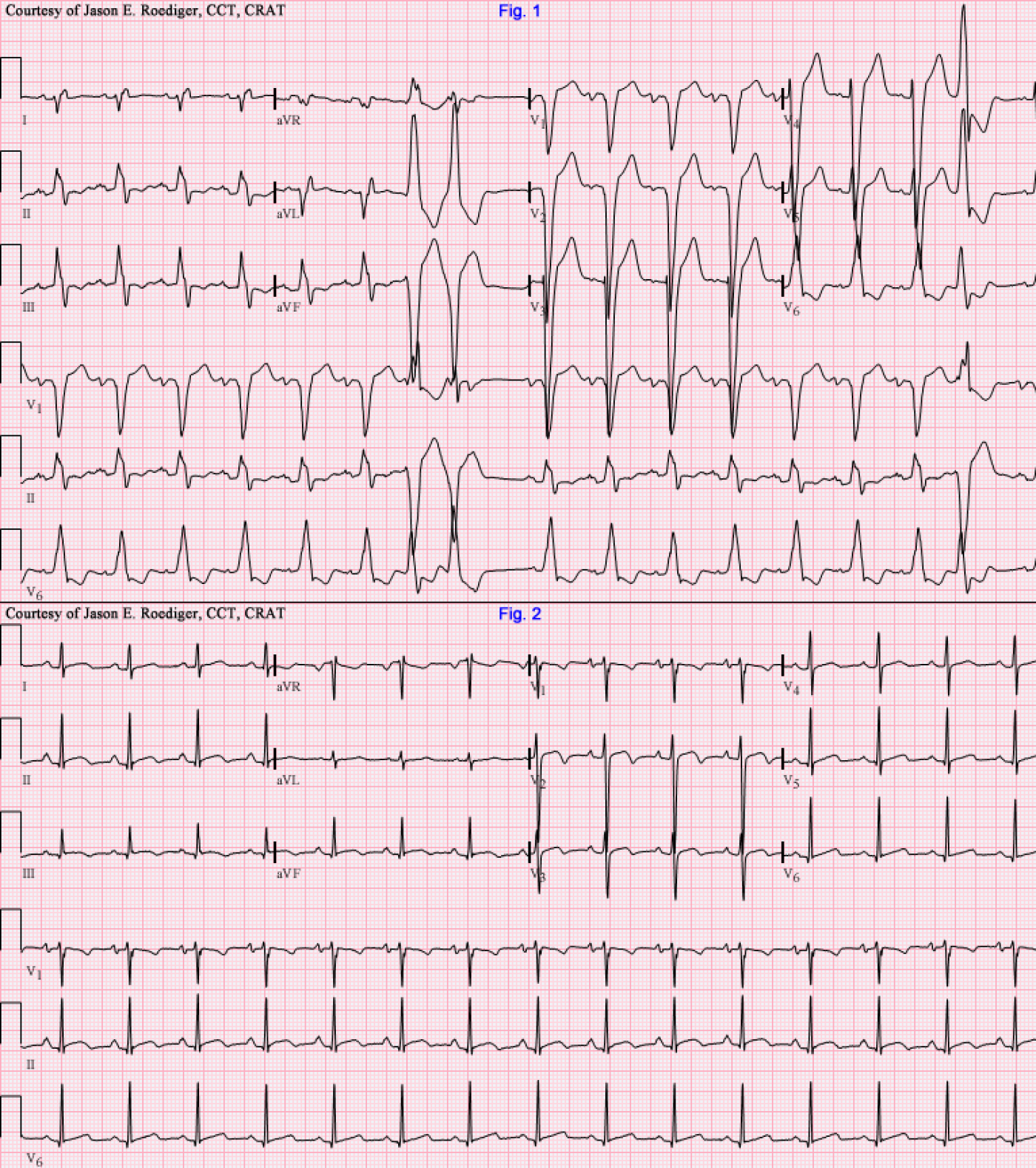
Fig. 2: This ECG was performed on a outpatient basis during a follow-up appointment with their physician. Have things improved or have they gotten worse?
QUESTIONS: In fig. 1, what rare combination of findings are present and what are those two findings highly suggestive of? What would explain the dramatic changes seen in Fig. 2?
HINT: Figures 1 and 2 both look dissimilar enough (esp. given the sequence in which they were recorded) that one might suspect they're from two completely different patients and technically that assumption would not be entirely wrong. Of what am I hinting towards? To be clear, both of these ECGs were performed on the same 49-year-old black male patient.
-
- jer5150's blog
- Log in or register to post comments
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
LBBB w/ RAD, perhaps
LBBB w/ RAD, perhaps idiopathic cardiomyopathy? Although given Fig 2 looks much better...some sort of congenital defect which has been repaired.
Christopher
sixlettervariable.blogspot.com
ems12lead.com
Rare combination of CLBBB and Right Axis Deviation
I agree with Christopher. This is a rare combination of CLBBB and RAD. This is seen mostly in DCMP or any cause of bivantricular failure. There is another hint of Biventricular failure is the low voltage QRS complexes in the limb leads compared to the chest leads. The BBB can be caused by delay in the LB or concealed retrograde penetration, in other words reversible and not permanent. There is evidence of LAE on ECG1. There is couplet in the middle of the tracing, the second was able to invade the AVN retorgradely and caused the following P not to conduct to the ventricle.
On ECG2 there is normalization of the QRS duration and no BBB. This is a result of appropriate diuretic treatment. There is no evidence of ischemia [no Qs] and the T wave changes may be T wave memory.
Another example
To see another example of LBBB with RAD, and Jason's comments, go to http://www.ekgguru.com/content/left-bundle-branch-block-almost-isoelectric-lead-ii
Thanks, Jason, for another great case study!
Dawn Altman, Admin
INTERPRETATION
Interpretation:
(1.) Sinus tachycardia (rate about 101/min) interrupted by . . .
(2.) . . . frequent multifocal ventricular premature beats (VPBs); both singly and in pairs.
(3.) Left bundle-branch block (LBBB)
(3.) Right axis deviation (RAD); here about 108°
(4.) Left atrial enlargement (LAE).
Comments:
This patient was diagnosed with congestive cardiomyopathy (CM). Undoubtedly, he would probably not be alive today had he not received an orthotopic heart transplant. Prior to his heart transplant, the vast majority of this patient's ECGs exhibited the same chronic combo of LBBB + RAD. Those select few ECGs that didn't show that pair, I would probably attribute to incorrect placement of the electrodes directly on the torso instead of on the actual extremities themselves. This is one of the biggest causes of false-positives for electrical axis. In one of Dr. Marriott's books, I've seen an ECG where a patient had both LBBB plus RAD but it was due to mirror-image dextrocardia and not CM.
Fig. 2
Interpretation:
(1.) Sinus rhythm (rate = 89/min)
Comments:
The nonspecific ST-T abnormalities are to be expected given the nature of this being a donor heart. A helpful clue in recognizing this as a transplanted heart would have been the presence of dissociated recipient P-waves from the native heart marching through but they are absent here. The tell-tale notching seen on the upstroke of the S-wave in lead V1 might be a very early sign of mild delay in the right bundle-branch (RBB). A significant majority of heart transplant patients go on to eventually develop full-blown RBBB. The irony, in this specific case, being that the patient had a LBBB in their native heart and will probably develop a RBBB in their donor heart. This would not qualify as an alternating bundle-branch block though.
Sources / References:
(1.) Nikolic G, Marriott HJ (Oct 1985). "Left bundle branch block with right axis deviation: a marker of congestive cardiomyopathy". J Electrocardiol 18 (4): 395-404. PMID 3906012.
(2.) Childers R, Lupovich S, Sochanski M, Konarzewska H. (2000). "Left bundle branch block and right axis deviation: a report of 36 cases". J Electrocardiol 33 (Suppl): 93-102. PMID 11265743.
(3.) Marriott HJL. Pearls & Pitfalls in Electrocardiography. 2nd ed. Baltimore: Williams & Wilkins, 1998, p. 114-115 & 156-159.
(4.) http://smj.sma.org.sg/3304/3304cr6.pdf
Jason E. Roediger - Certified Cardiographic Technician (CCT)
[email protected]
Great to see.
Also Alcoholic Cardiomyopathy will cause LBBB with RAD.
Txs.
MM
Thank you
Nice case.
Terminology: LBBB vs IVCD?
NICE case history and follow-up in this case by Jason! I'll add a few points in support of the very interesting explanation.
Experts might disagree on terminology of the conduction defect present in the TOP tracing. Those who classify RBBB and LBBB based primarily on precordial lead appearance would term this LBBB. One cannot argue with this functional terminology. Others (my preference) - reserve definition of "LBBB" and "RBBB" to need for fulfilling criteria in all 12-leads. For them, rather than "LBBB" - a designation of IVCD (IntraVentricular Conduction Defect) is more befitting given clearly atypical QRS morphology in lead I of this tracing for LBBB.
The septum is normally depolarized from left-to-right. This left septal component is lost with typical LBBB (since block of the left bundle results in initial depolarization of the septum down the right side via intact right bundle). Ventricular depolarization with typical LBBB is therefore essentially all in right-to-left direction - and this should result in a monophasic upward R in lead I similar to what is seen in V6. Clearly - something beyond simple LBBB must have occurred in this patient to produce this atypical pattern in lead I (be that superimposed infarction, valvular disease, scarring from cardiomyopathy or combination thereof).
BOTTOM LINE: Whether one calls the conduction defect in the TOP tracing "LBBB" - "atypical LBBB" - "LBBB in precordial leads with RAD" "IVCD" (my preference) - or "IVCD with RAD" relates to semantics of one's preference for terminology. A case can be made for each term. Jason emphasized the essential point - namely, that this TOP ECG (esp. in context with associated LAE, probable LVH [very deep S waves in V2,V3] and ventricular ectopy) strongly suggests the underlying presence of significant cardiomyopathy. Fortunately the patient received a new heart.
THANKS Jason for presenting this interesting case!
REFERENCES (More on Conduction Defects): My web page on Bundle Branch Block -
Ken Grauer, MD www.kg-ekgpress.com [email protected]