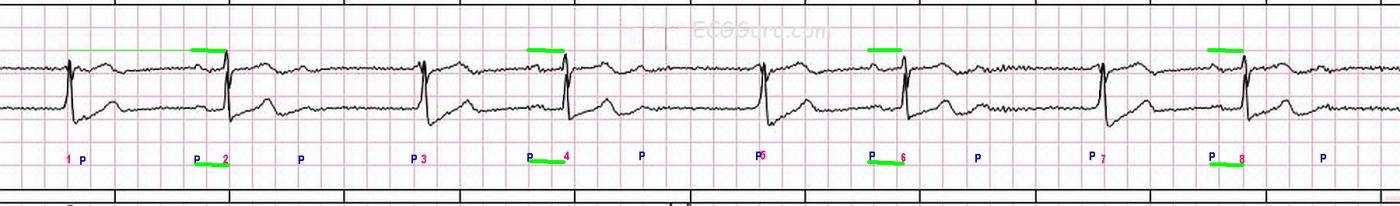
This strip was obtained from a woman who presented to her doctor’s office with hypertension. While there is some artifact in the baseline, it is possible to determine the presence of P waves, thanks in part to having two leads to assess. We have provided an unmarked version of the strip for you to use, and also a marked version for the sake of this discussion.
The underlying rhythm is sinus bradycardia, at about 60 bpm, but with some slight variation in the P to P intervals (about 920 ms to 1040 ms). Because of the artifact, it is difficult to determine the exact P to P intervals, and the exact morphology of the P waves. So, we can’t say for sure that the P waves are all alike.
The AV block occurs at a 3:1 ratio. That is, for every three P waves, one is conducted and produces a QRS complex. When the P waves are not conducted, an escape rhythm occurs.
The escape rhythm occurs at an escape interval of about 1720 ms. In other words, when a QRS does not occur by that time, the escape beat is produced. It appears to be from the AV junction, in spite of the slow rate, because the escape QRSs look like the sinus conducted QRSs. Both sinus and junctional rhythms are conducted along the bundle branches and produce the same QRS morphology. The QRS complexes are approximately .08-.10 seconds wide. Note that QRS complexes numbered 3, 5, and 7 have a P wave fused to the beginning of the QRS, making the QRS look wide when it is not. A junctional escape rhythm results from AV block in the AV node, as the junction is the first available pacemaker below the AVN.
This patient was scheduled for a treadmill stress test in her doctor’s office, which was cancelled. She had no cardiac symptoms at the time of the ECG, except the above-noted hypertension. Unexplained bradycardia, especially when accompanied by AV node blocks, should trigger an assessment for inferior wall M.I., since the inferior wall of the LV shares a blood supply with the SA and AV nodes in the majority of people.
Whether an AV block is "second-degree" or "third-degree" may not matter as much as WHERE the block is and what the resulting rate is. If the block is in the AV node, as opposed to the bundle branches or lower His bundle, the patient will have the benefit of a junctional escape rather than a ventricular escape rhythm. AV node level blocks tend to be temporary and reversible, while sub-Hisian blocks can be more permanent and more life-threatening. The rate, and the cardiac output, matter more to the patient than the "degree". Should the rate be so slow that the patient loses perfusion, a pacemaker may be required to increase it.
Our thanks to Palm Beach Gardens Fire Rescue for donating this strip.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.



Comments
Is this Really High-Grade AV Block?
Fascinating tracing — that I will provide an alternate explanation for. Thanks to Dawn for labeling this tracing. There is group beating (alternating long-short intervals) — with fairly regular P-P intervals (underlying sinus arrhythmia and/or ventriculophasic sinus arrhythmia as a result of the AV block). As per Dawn — the underlying atrial rate ~60/minute — and the PR interval preceding the 2nd, 4th, 6th and 8th beats is constant. This confirms that there IS some conduction, albeit with a long PR interval (1st degree AV block). Beats #1,3,5,7 are escape beats.
Interesting case — with LOTS of great points for clinical discussion!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Great comments, Dr. Ken, thank you.
We are actually in agreement on all points you have made, except perhaps the definition of "high-grade AVB" I have always considered any second-degree AVB (Type I or Type I, to be "high grade" of conduction is 3:2 or less and a bradycardia results. Maybe it's time for me to reconsider my use of this term .
What I am probably most guilty of here is oversimplification i use the "ECG Basics" format to present rhythm strips for teachers and students of basic level ECG classes I hope they are suitable for most beginners. That being said, I do agree that the underlying block here is probably Type I, simply because it occirs at the level of the AV node. We would, of course, need to see two consecutive P waves conducted to see the progressive prolongation of the PR interval.
Without a 12-lead ECG, or EP studies, there is much we can't be sure of anyway, but it makes for a great discussion. The escape rhythm might very well originate from the His bundle. But in basic ECG classes, if the QRS is the same in the conducted beats and the escape beats, the answer on the multiple-choice test is always going to be "junctional escape". The level and permanency of the lesion would, of course, determine the definitive treatment. But many of our readers are emergency workers or bedside caregivers whose first consideration should be rate and hemodynamic response to the rate, regardless of the etiology of the rhythm. That is, a Wenckebach block with a very slow rate could be more symptomatic than a third-degree AVB, and the patient response should be addressed first.
This is a reference I have used for many years for my definition of "high grade"
https://lifeinthefastlane.com/ecg-library/basics/high-grade-block/
Thank you (as always) for your thought-provoking comments. We are so fortunate to have your input on the ECG Guru!
Dawn Altman, Admin
Escape-capture bigeminy
ECG GURU Vince DiGiulio pointed out on the ECG Guru Facebook page that this is also an example of "Escape-Capture Bigeminy", which it is. Now I want to take a vote:keeping in mind this was intended for basic-level readers, I would like to re-title this post. What do you think?
Dawn Altman, Admin
Do P Waves Have a Chance to Conduct?
This is an excellent post not only because of the very interesting rhythm and the clinical questions that it raises — but equally so because of the points it raises about teaching others rhythm interpretation. Regardless of the interpretation level of the provider — it is essential to appreciate that QRS morphology of every-other-beat here is NOT the same — and that without a 12-lead tracing, we really have NO idea of from where the escape focus is arising (sometimes ventricular beats may look very similar to sinus beats if all you have is a single lead).
As to defining Mobitz I vs Mobitz II vs High-Grade AV Block — the KEY concept that is so often overlooked, is that before you can judge degree of AV block, one needs to assess IF P waves fail to conduct DESPITE having a chance to do so. That concept is unfortunately also missing from the LITFL link that Dawn cites. In the fascinating rhythm strip that Dawn presents here — it is because we never see 2 conducted beats in a row AND because we never see 2 non-conducted P waves in a row that SHOULD conduct but fail to conduct, that we cannot be certain about the nature of the AV block. That said, as an admittedly more advanced concept — we should recognize GROUP beating — and, knowing that the overwhelming majority of 2nd-degree AV blocks are Mobitz I (over 95% in my experience) — surmise that this rhythm probably represents Mobitz I.
At the least — all providers should recognize that there is some degree of AV block here — but that because there IS some conduction, this cannot be complete AV block. They should recognize the importance of knowing the clinical situation (this patient apparently was not hemodynamically unstable) —in which case inquiring about the patient's medication, and a search for reasons why there is bradycardia rise to the forefront. In summary, there are numerous Pearls for providers of any level to glean from this case — culminating in recognition of the "escape-capture" form of bigeminy pointed out by Vince. THANKS to Dawn for presenting this case!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
re: nice strip
Interesting strip indeed. Regarding escape-capture, I believe it was used in the setting of extreme sinus bradycardia that the junction escapes and when the sinus beat occur then it captures the ventricles. Second, I think the term advanced heart block was coined (like 2nd AVB 2:1) because of some difficulty of the certainty of identifying what is the phenomenon behind the AHB. A 3:1, 4:1 etc can occur in the setting of a type I or type II 2nd AVB. It seems there is a bit similar strip in Chou's. During the events of some ventricular captures, the dominant rhythm is maintained by subsidiary pacemakers. In this case, we are not sure if the pattern is coincidnetal or a latter pattern will occur. Very nice strip. I believe I have a similar tracing around.
REPLY: to Dr Arnel’s Comment
Thanks as always for your comments Arnel! I’d like to address them. I believe we DO have bradycardia here as part of the initial problem — which results in the escape beat — which is then followed by the next on-time sinus P wave that results in sinus capture (ie, “escape-capture”). Otherwise — we have not been discussing “advanced heart block” — but rather the issue of whether or not there is “high-grade AV block”. I’ve never liked the term “advanced heart block” — because I think it can be confusing as to what is truly meant ... In contrast, the term “high-grade AV block” is (in my opinion) a very functional one, because it suggests that repetitive P waves that should conduct are not conducting. As you and I state — nonconduction of successive P waves may be due to either Mobitz I or Mobitz II 2nd-Degree AV Block. But the KEY point about this definition is that successive P waves FAIL to conduct DESPITE having adequate opportunity to do so. This is NOT the case here — because the 2nd P wave coincides with the onset of the escape beat QRS, therefore having a PR interval too short to be able to conduct. Therefore, we NEVER demonstrate failed conduction by successive P waves, because the 2nd P wave never “has a chance” to conduct. That’s why it remains entirely possible that we are merely dealing with Mobitz I being exacerbated by bradycardia that is potentially (at least in part) reversible by something as simple as withholding potentially rate-slowing medication ... BOTTOM LINE: The key point I am trying to make is that we really have NO idea as to how severe the AV block in this case is or is not ... THANKS again Arnel for your comments, which have nicely contributed to our discussion!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Great discussion
Thanks, Drs. Arnel and Ken,
I understand and agree with your comments about the severity of this block. I take it to be mostly innocuous and most likely Type I exacerbated by the underlying bradycardia. Because the patient was well-perfused, I don't see an emergency here, just an opportunity to reevaluate her meds and keep an eye on her. I think my BIGGEST problems are 1) I should not have presented this in the "ECG Basics" column and 2) I fell back on the term "high-grade", which should be reserved for clinically worrisome blocks where P waves that should have conducted, didn't - preferably when two P waves in a row don't conduct.
What I would like to ask you - and any other ECG Gurus out there, is - please help me re-name this post! If anything ever needed a new nam, this one does! Thanks in advance.
Dawn Altman, Admin
Proposed New Names for this Post ...
How 'bout changing the name to "ECG Rhythms"? — OR — You could say something like "ECG Rhythms for Teaching or Learning". I favor the 1st title, because it is "short and sweet", and this is really what this post is about. The 2nd title might also work — since sometimes you use more "basic" rhythms — and other times the rhythms are more advanced. ALL these rhythms are good for teaching — and the more complex cases (like the rhythm for this current thread) are also good "learning" cases even for advanced providers (who may be teachers for those on their staff).
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Question for Dr. Ken
Of course, I see the difference in QRS morphology in every other beat, but I attributed it to the P waves present at the beginning of each wider QRS. What else am I missing? Is the slightly wider S waves?
Dawn Altman, Admin
The Difference in QRS Morphology between Odd-Even Beats
DAWN — Regarding your question about the difference in QRS morphology, beats #1, 3, 5 and 7 in the Top tracing to me look different than beats #2, 4 and 6. That is, the odd-numbered beats show a smaller and thinner R wave that I believe is not affected by superposition of the neighboring P wave. In contrast — the difference we see in QRS morphology for the Bottom tracing may be influenced by the superimposed P wave. But note how much smaller in amplitude the P waves are in this Bottom tracing — so I suspect there still IS some difference in QRS morphology here. But in the Top tracing, there should be little doubt that odd beats manifest a different QRS than even beats. How different this truly is I believe can only be determined by getting a 12-lead … Hope that answers your question!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Thanks, Dr. Ken
I do see the difference in QRS morphology. Guess I was paying too much attention to the bottom strip. Regarding the name of the post, I am removing the word "basic" now, but I need a name for this rhythm so it can be searched accurately. Many thanks!
Dawn Altman, Admin
re: AHB discussion in twitterverse
Would like to share a short conversation on AHB in twitterverse.
https://twitter.com/naderjo/status/934728499344134144
My Final Thought Regarding Dr. Arnel Comments
Thanks for your latest Comment Arnel, in which you invited us to the conversation at the link your provide. Others may have used the term, "Advanced AV Block". All I am saying is that I do not like that term — because I believe it is confusing. As I've detailed in my Comments on this thread — it IS possible that some forms of Mobitz I 2nd-Degree AV Block may be classified by those others as "advanced" block, because more than 1 P wave in a row may be nonconducted — but, the clinical reality is that such AV block is not necessarily "advanced" (and may not necessarily need pacing). Use of the term "high grade" in my opinion better reflects the fact that more than 1 P wave in a row that should conduct, does not conduct. To my reading of the conversation you cite on twitterverse (above) — commenters on that site are not fully aware of the clause in my definition that is KEY, namely that before you classify AV block as "high-grade" — it is essential to demonstrate that there HAS BEEN adequate opportunity for conduction of the P waves that did not conduct. Otherwise, under other circumstances (ie, with less underlying bradycardia) — successive P waves will not go unconducted without any change in the severity of the existing AV block. Alas, I merely state my opinion. I realize not all agree with me, which is fine — :)
Ken Grauer, MD www.kg-ekgpress.com [email protected]