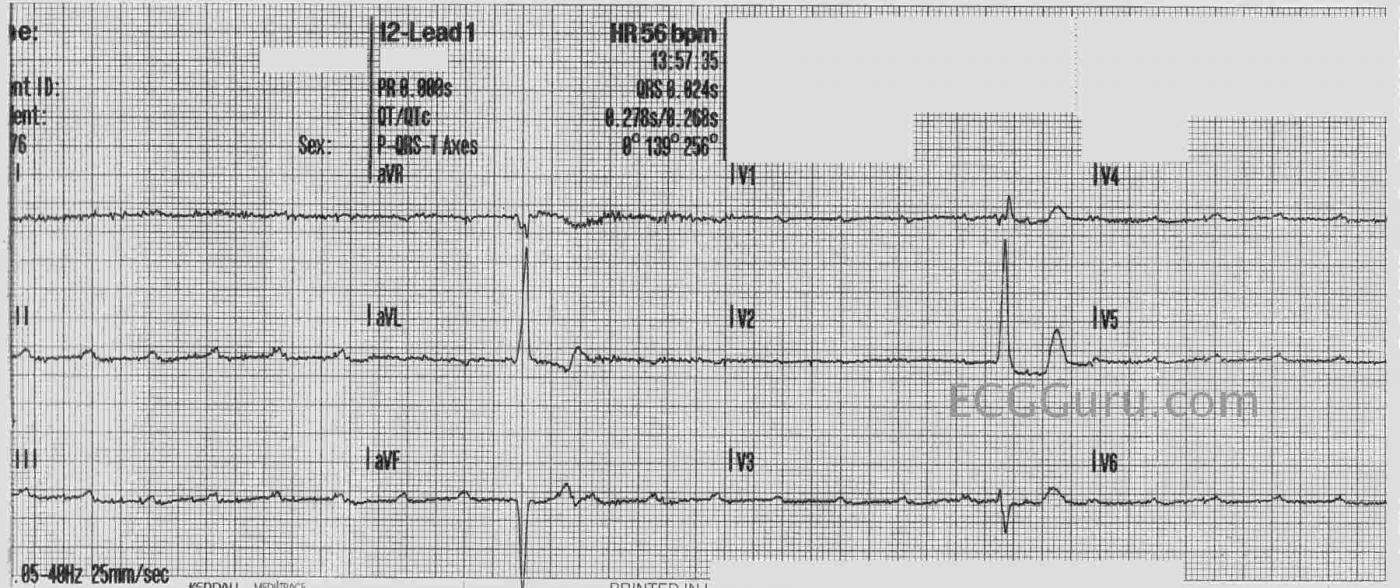
The Patient This ECG was obtained from a 76-year-old woman who had just lost responsiveness while under care of an EMS crew. This tracing was obtained before a trans-cutaneous pacemaker was applied.
The ECG The most noticeable feature of this ECG is the extremely slow rate. In fact, there are only two QRS complexes visible. The P waves are regular at a rate of about 145 bpm, so the underlying rhythm is sinus tachycardia. NONE of the P waves are conducted, as evidenced by the different “PR intervals” in the two QRS complexes seen. This is complete heart block at it’s most extreme – the QRS complexes represent a very insufficient escape rhythm. A pacemaker is the only immediate treatment for this rhythm. Unfortunately, we don’t know the outcome for this patient.
It is very difficult to make judgements about the QRS complexes with only two of them, visible in three leads each. The first set show the criteria for left ventricular hypertrophy. The QRS in aVL is 20 mm tall, and anything over 11 mm meets voltage criteria for LVH. In addition, the ST segments have the “strain” pattern, another sign of LVH. The second QRS complexes are not typical of a normal ECG or one with LVH. We cannot vouch for the precordial lead placement.
There is some disagreement in the literature regarding the naming of the blocks. Some consider “high-grade” to be only second-degree AVB with two or more consecutive non-conducted P waves. Others include third-degree AVB in the “high-grade” category. It can come down to just semantics – the RATE and how the patient responds to the rate is the primary consideration. Classification as to the origin of the block is helpful when determining the best long-term treatment decisions.
This is a good ECG for teaching the concept of AV dissociation, and how dangerous third-degree AV blocks and high-grade second-degree AV blocks can be.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Impending Ventricular Standstill
As I know Dawn suspected — the major area of discussion about this tracing lies with terminology. Dawn has described the findings = underlying sinus bradycardia with just 2 QRS complexes in the slightly less than 10 seconds of monitoring. My thoughts are as follows:
— I don’t know for sure what the rhythm is. For lack of a better term — I’d call this impending ventricular standstill. I would not call this complete AV block — because there is no reliable ventricular rhythm. In fact, we have NO idea of what the next 10 seconds of monitoring would show (ie, there may or may not ever be another QRS complex ... ).
— I would not speculate on LVH and/or LV “strain”. Given no relation of P waves to either QRS complex in this tracing — neither beat is conducted. Therefore, we have NO idea from where these beats originate. Both are wide — and these could be ventricular escape beats in a failing heart, rather than originating from within the conduction system. Therefore, criteria for chamber enlargement are not valid.
— Regardless of how you classify this rhythm (and regardless of whether the next 10 seconds of monitoring do or do not reveal another QRS complex) — Dawn is correct in assessing this as a critical bradyarrhythmia with urgent need for cardiac pacing.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
A Very Dangerous Rhythm
Dawn...
This is a great teaching case!
If I had to choose a name for this horrible rhythm, I would call it a paroxysmal tachycardia-dependent AV block (TD-PAVB). The P waves look sinus and the rate could be due to loss of BP support with hypotension. Or, it could be an atrial tachycardia coming from a site immediately adjacent to the sinus node. Six of one - half-dozen of the other.
The issue here is that the markedly decreased P-P intervals are causing the P waves to enter the AV node during the refractory period left by the previous P wave because the AV refractory period is longer than the P-P interval. The AV block is likely due to concealed conduction by the atrial impulses into the AV node.
Paroxysmal AV block, whether it's pause-dependent or tachycardia-dependent, always occurs in hearts with very diseased conduction systems. It does NOT occur in normal hearts. That's why the ventricular escape response is so inadequate. When we encounter a 3rd degree AV block, most of us are used to seeing a sinus rate of about 70 and a ventricular rate anywhere between 20 and 50. In such cases the challenge is always determining whether the resulting AV dissociation is pure AV dissociation or AV dissociation due to 3rd degree AV block.
Not so with PAVB! This ECG demonstrates classic PAVB! If one cannot see the obvious 3rd degree AV block and the imminent danger it presents to the patient, then I would suggest a visit to an ophthalmologist!
You can certainly see temporary 3rd degree AV blocks of the more typical kind following an inferior MI. Usually they are short-lasting and the escape rhythm tends to be a life-sustaining junctional rhythm or a ventricular escape rhythm in the 40's or so. Those 3rd degree AV blocks rarely kill (but, of course, they certainly CAN kill).
PAVB is the type of block that kills very quickly due to the sudden onset and lack of sufficient escape rhythm. I take it from your history that the onset of this event occurred in the presence of the paramedic team. That is the only reason she is alive today.
PAVB can present with only a couple of non-conducted P waves. Those cases are often called a high-grade Mobitz II. Whatever... they also need a pacemaker immediately.
The bottom line is that I agree with both you and Dr. Grauer that 3rd degree AV block is going to require pacemaker support - no matter what you choose to call it. In some cases it will be temporary but in most it will be permanent. My point here is that this is the type that is most likely to kill immediately.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
PAVB (Paroxysmal AV Block) - Pause or Tachycia Dependent
THANKS so much for your comment Jerry. I had not been aware of the concept of PAVB. We all agree on immediate need for pacing — but helpful to add your wonderful insights to our understanding! — :)
Ken Grauer, MD www.kg-ekgpress.com [email protected]
New term for me, too.
Thanks, Dr. Jones. I now have a new term to explain a phenomenon I've seen more than a few times. I always attributed the sinus tach to a sympathetic response to loss of perfusion, but didn't really sort out the way the tachycardia could contribute to the AV block. I don't have any information from beyond the emergency dept phase of this case, but highly doubt that the patient lived much longer. Thanks again for your insight.
Dawn Altman, Admin
PAVB
Thanks for the kind words, Ken and Dawn. PAVB is often referred to in the older literature as Phase 3 block and Phase 4 block.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd