If you are an ECG instructor, you probably carefully choose ECGs to illustrate the topic you are teaching. One of the reasons for the existence of the ECG Guru website is our desire to provide lots of such illustrations for you to choose from.
Sometimes, though, an ECG does not clearly illustrate one specific dysrhythmia well, because the interpretation of the ECG depends on so many other factors. In order to get it “right”, we would need to know information about the patient’s history, presentation, lab results, or previous ECGs. We might need to see the ECG done immediately before or after the one we are looking at. Some ECG findings must ultimately be confirmed by an electrophysiology study before we can know for sure what is going on.
For those of us who are “ECG nerds”, it can be fun to debate our opinions and even more fun to hear from wiser, more advanced practitioners about their interpretations.
My belief, as a clinical instructor, is that we must teach strategies for treating the patient who has a “controversial” ECG that take into account the level of the practitioner, the care setting, and the patient’s hemodynamic status. In some settings, it might be absolutely forbidden for a first-responder to cardiovert atrial fibrillation, for example. But atrial fib is routinely cardioverted under controlled conditions in hospitals. The general rule followed by emergency providers that “all wide-complex tachycardias are v tach until proven otherwise” has no doubt prevented deaths in situations where care providers did not agree on the origin of the tachycardia.
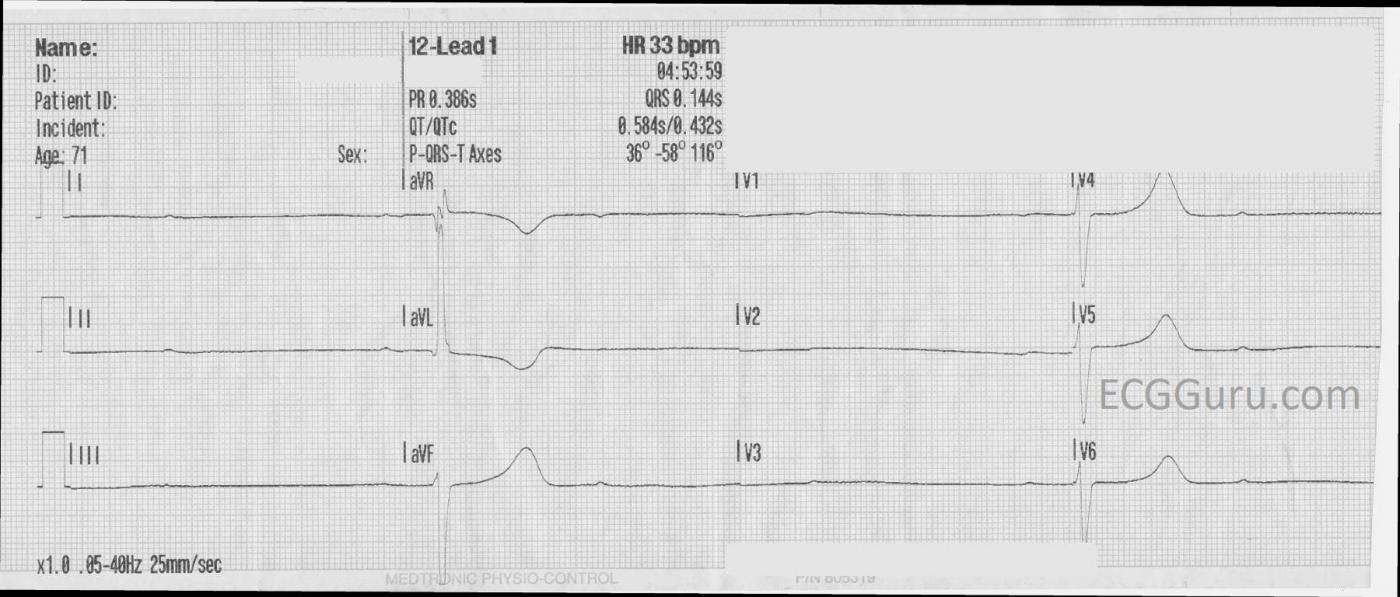
The ECG: We do not have much patient information to go with this ECG, just that it is from a 71-year-old woman who developed severe hypotension and lost consciousness, but was revived with transcutaneous pacing. Here is what we do know about this ECG:
· There are regular P waves, at a rate of about 39 bpm (sinus bradycardia).
· There are only two QRS complexes, shown in a total of six leads, and the rate is 13 bpm.
· The two PR intervals that are seen are the same at 368 ms, or .368 seconds (first-degree AVB).
· There are three P waves for every QRS complex. (second-degree AVB, Type II).
· The QRS complexes are 144 ms wide (.14 seconds).
· The QRS morphology cannot be evaluated in 12 leads here, but the pattern is consistent with right bundle branch block and left anterior fascicular block (bifascicular block). Were we at the bedside, another 10 seconds of 12-lead ECG might produce a QRS that falls into the remaining leads’ sections of the tracing.
It would be very important to determine what caused the severe slowing of conduction. The paper speed has not been altered, and that should be ruled out whenever all rates and intervals are prolonged. The severe sinus bradycardia, second-degree AVB, first-degree AVB, and bundle branch block all point to a global cause of poor conduction. Electrolytes, drugs, vagal stimulation, possible acute M.I. – all of these need to be assessed. And, eventually, the best definitive treatment will need to be decided.
But what is the MOST IMPORTANT issue here? The RATE! And the patient’s response to the extremely slow rate. Before we spend any time on the cause or treatment, we must address the rate and the patient’s hemodynamic status. A transcutaneous pacemaker, if available, is called for. CPR may be needed until the pacemaker can provide a perfusing rate. Rate-enhancing drugs may be used, and temporary transvenous pacing. If the patient’s perfusion status is not addressed, the rest will not matter.
When students are taking an ECG class, they most often want to know, “what is the name of this rhythm?” and “what are some shortcuts or mnemonics I can use to remember the names of the rhythms?”. They will be distressed if the instructor says, “This could be second-degree AVB, or we could call it high-grade AVB, or a longer strip might show it to be third-degree AVB.” The instructor may even feel distressed by not knowing “for sure.” But (and this is admittedly an editorial on my part), I think we do our students a disservice to lead them to believe that there is a “right” answer to every ECG strip. They need to know that some ECGs cannot and should not be read in a vacuum, but rather in light of the patient’s information. They need to know that comparison with a previous ECG, or adding additional leads, or running a longer strip may illuminate the problem. But most of all, they should understand what immediate actions can safely be taken until we do “know for sure”.
We welcome your comments on this topic, whether you are a teacher, a student, a provider, or all of these.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Be Systematic — The "Answer" Comes After This ...
Interesting topic of discussion by Dawn. Regarding the rhythm shown above — I’m less confident about what I’m seeing. P waves are of extremely small amplitude. I’m not sure there is a regular atrial rhythm. I’m not convinced given that we only see 2 beats that there is conduction rather than a very slow ventricular escape site. But then again — NONE of this matters — since as per Dawn, the primary problem is profound bradycardia — and the immediate treatment need is pacing. Nothing else matters until pacing is accomplished — after which one can get more history and monitor the patient’s clinical response.
As to the question about what a particular ECG shows — Dawn’s discussion is precisely the reason that I always emphasize a systematic approach. A precise rhythm or 12-lead ECG diagnosis is not always possible. What counts more is a systematic approach in which specific findings are determined (ie, presence of atrial activity, QRS width, rate, regularity, relation of P waves to QRS complexes if assessing a rhythm — and adding for a 12-lead assessment intervals, axis, chamber enlargement and QRST changes) + correlation to the clinical history + determining what (if anything) needs to be done at his time for the patient. Attaining a specific rhythm or 12-lead ECG diagnosis need not take priority to the above steps. Focusing too much too soon on a specific diagnosis risks premature closure — with the patient not being adequately cared for as an undesired side effect.
Ken Grauer, MD www.kg-ekgpress.com [email protected]