The patient: This ECG was taken from a 66-year-old man who was complaining of chest pain at rest. He had been previously diagnosed with lung cancer with metastases to his bones. The last ECG, taken one week ago, was normal.
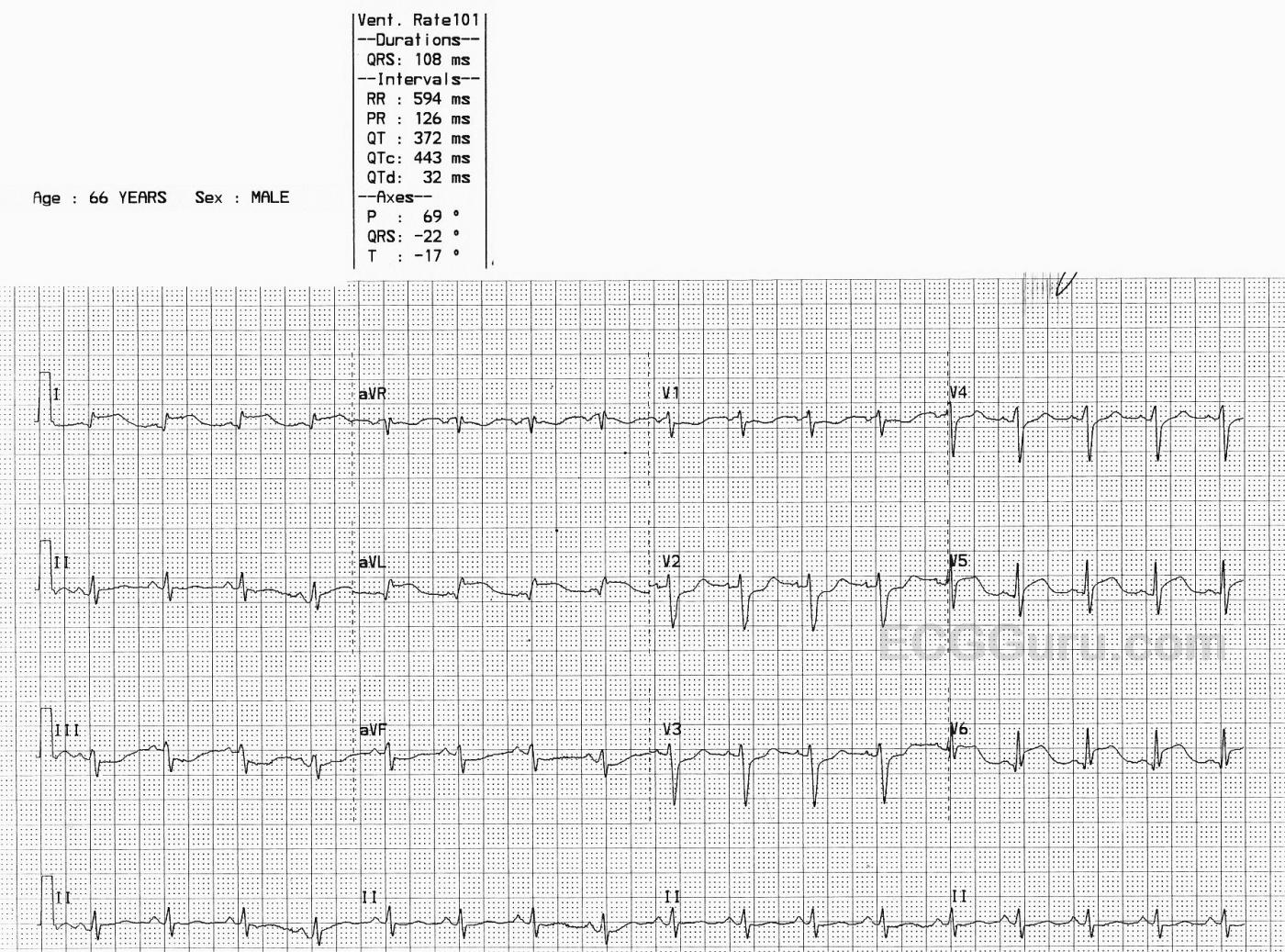
The ECG: There is mild sinus tachycardia at 101 bpm. The rhythm is regular. The QRS duration and PR interval are normal, as is the QTc. The QRS voltage in the limb leads is small, and we do not know the patient’s height and weight.
There are notable ST elevations in I and aVL (high lateral wall) and in V5 and V6 (low lateral wall). When the high and low lateral walls are similarly affected, we usually look to the circumflex artery as the culprit artery. We also see ST depression in Leads III and aVF (reciprocal to the STE in I and aVL) and in V1 – V4. This could indicate subendocardial damage or reciprocal changes. This ECG meets the criteria for acute lateral myocardial infarction.
The patient was taken to the cath lab emergently. His coronary arteries, including the left circumflex, all were free of occlusive lesions. He had no coronary spasm during the procedure, but it was decided that spasm had been the cause of the ECG changes. His ECG reverted to normal.
It is important to record abnormal findings, as some changes can be temporary or fleeting. Coronary artery spasm can cause ischemia and damage to the heart, just as plaque lesions and blood clots can.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute STEMI that Wasn't? (What is the Answer?)
Fascinating case presented by Dawn. The ECG shows sinus tachycardia at ~100/minute — normal PR interval – borderline QRS duration (0.10 second) — and what looks like some QTc prolongation (difficult to accurately assess given the fast heart rate). No chamber enlargement.
Dawn has noted the remarkable findings. I'll add that not only are there acute ST elevations in all lateral leads (I, aVL, V5, V6) — but Q waves are already established in these leads. Mirror-image opposite ST depression to the ST elevation in aVL — is seen in lead III (with lesser degree of reciprocal change in the other inferior leads).
There is also "shelf-like" ST depression in lead V2 (with lesser ST depression in leads V1-V2) — so clearly an ECG that in association with the history of "chest pain" — is diagnostic of an acute ongoing posterolateral STEMI, presumably from LCx (Left Circumflex) occlusion as the "culprit" artery.
Yet the cath was reported as normal!
Pure coronary spasm is not a common entity in a 66-year old patient. In theory — one wouldn't expect Q waves in association with a transient episode such as this one — but "anything is possible" — and even large Q waves have been shown on occasion to develop within 1-2 hours of infarction — and also to quickly resolve.
I have questions that are unanswered by this case. Because it is so totally unexpected to find no evidence of acute infarction on the cath of this patient — I'd really want to know the following:
i) We are told that the cath report was, "free of occlusive lesions" — but we were not told if there was any evidence on underlying coronary disease.
ii) Did this patient have any history of prior heart disease? Of chest pain? Of transient severe chest pain episodes that spontaneously reolved — which may have suggested prior spasm episodes?
iii) Was troponin done? Elevated?
iv) We are not told of the details of the timing of associated events. The last previous ECG was done a week earlier and reported as normal. Then this patient "complained of chest pain at rest". But how long before this ECG was taken was it that this chest pain began? How long did it take for the "emergent cath" to be done? Was the patient's chest pain constant throughout the entire episode — or did it resolve prior to cath? If so — how much time prior to cath?
This case is fascinating in how it is puzzling. Perhaps coronary spasm was the diagnosis. However, without any demonstration of this during the cath procedure — I am not convinced given details of the case. It is possible for there to be brief coronary occlusion that spontaneously resolves fast enough for even high sensitivity troponin not to rise — in which case I wonder if that could be an answer? But without answers to the questions I pose above — I maintain that we do not really know what happened in this case.
That said — this is a great tracing to "hone" your ECG interpretation skills on!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Perplexing ECG with Excellent Comments by Dawn and Ken
I certainly agree with both Dawn and Ken. I really don't have any comments other than to expand a bit on the Q waves that Ken mentioned.
The q wave in V6 is very small and too narrow to be considered pathological. I think it is simply a septal q that one would expect to see there. While I would also expect to see septal q waves in Leads I and aVL, the q waves in those leads are certainly too wide to be considered septal. As Ken pointed out, Q (or q) waves can appear very shortly after the onset of chest pain and then disappear with resolution of the ischemia. I've seen that happen several times. Here is the reason that happens:
Conduction in the ischemic region is slowed. This allows the recording electrode overlying the ischemia to detect the faster onset of depolarization in the opposing, non-ischemic area of the heart. Of course, it perceives that vector as traveling away from it, so it begins to record a negative deflection (the Q wave). However, conduction in the ischemic region now catches up and the R wave is inscribed, overriding the oppositely-directed initial vector. This certainly does not happen in every case, but that is - in my opinion - the best explanation I've found so far.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Helpful explanation
Dawn Altman, Admin
Thanks, Dawn!
Thanks for your comment!
My understanding is that the Q waves due to conduction delay in the ischemic area will remain as long as the ischemia persists. With resolution of the ischemia (spontaneously, through thrombolysis or PCI), conduction in the ischemic area improves and the Q waves will disappear. They are based on the difference in the conduction velocities in the ischemic area and the other (likely reciprocal) non-ischemic areas of the heart. They are not due to infarcted tissue.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd