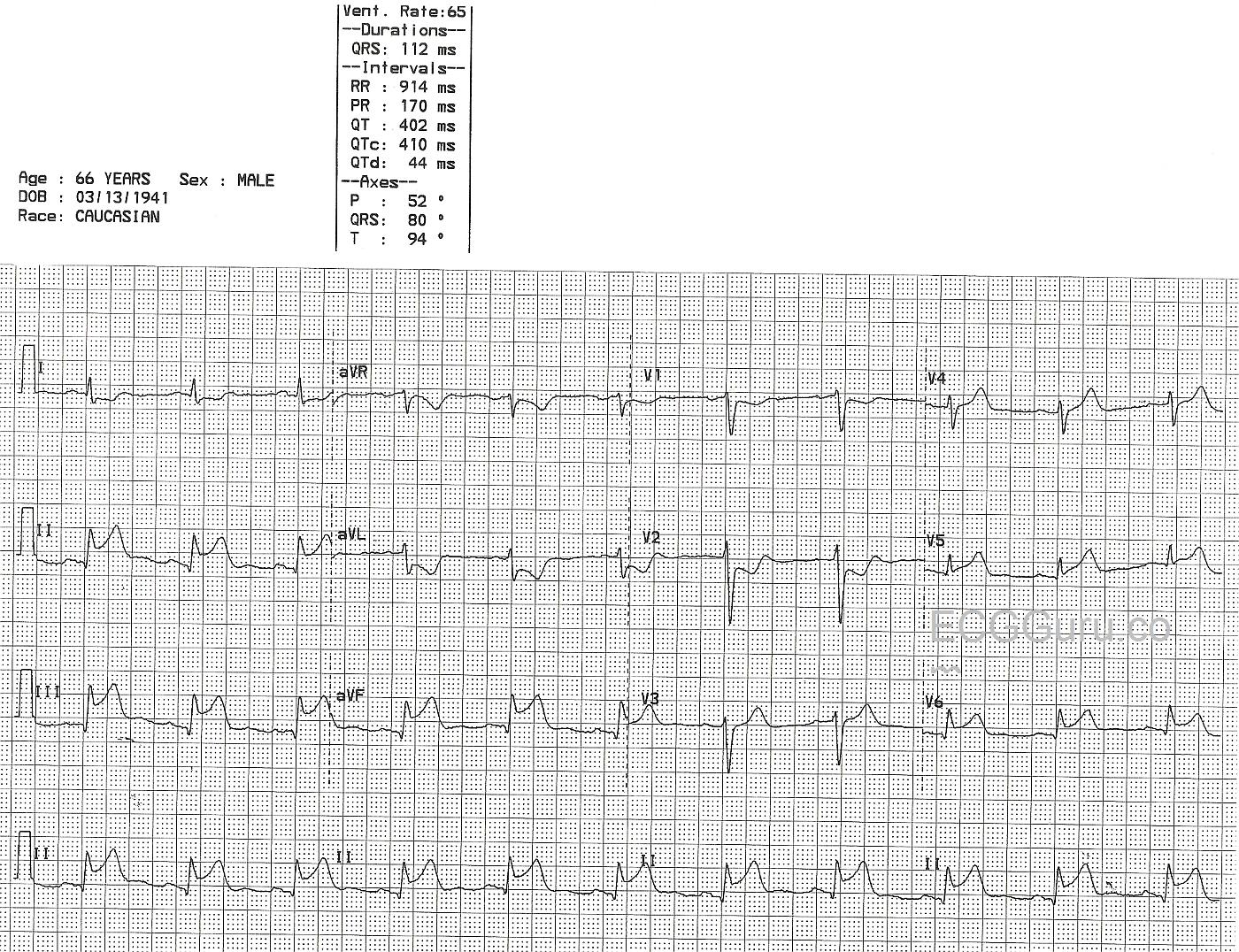
This 66-year-old man presented with a complaint of chest pain. His ECG shows a "classic" inferior wall ST-elevation M.I. (STEMI). The ST elevation is apparent in Leads II, III, and aVF, which are the leads that reflect the inferior wall of the left ventricle. In addition, this ECG shows ST elevation in Leads V5 and V6, the low lateral wall. The ST depression in V1 and V2 are reciprocal changes caused by acute injury in the posterior wall. In the majority, the RCA supplies the inferior-posterior wall, the right ventricle, the right atrium (including the SA node and the AV node), and in some, the low lateral wall. The proximal location of this man's occlusive lesion has caused damage in all these areas. The relatively slow rate is common in IWMI and can be caused by SA node injury, vagal stimulation, or medications. Clinical data is not available for this patient.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
RCA infarct
Nice example of a proximal RCA occlussion. For confirmation of RV involvement you can consider right sided leads. These proximal RCA infarcts are often complicated by rhythm disturbances, most commonly AV block of varying degrees. For this reason during the setting of primary PCI you have to be prepared for temporary pacing which can be discontinued once the restored flow down the RCA has corrected the arrhythmia.
Dr Stasinos Theodorou
MB ChB, MRCP(UK)Interventional Cardiologist
www.cardiolimassol.com
RV involvement
Just a question: how can we tell from this ECG that there is RV invlovement? To me, it just looks like an inferolateral MI.
Dave R
My Guess Would Be NO RV Involvement ...
My guess would be that there is no RV involvement in this patient - given the lack of any hint of ST elevation in lead V1 with an ECG picture otherwise totally consistent with acute infero-posterior STEMI. As per Dr. Theodorou - confirmation would be forthcoming with use of right-sided leads (esp. lead V4R).
Ken Grauer, MD www.kg-ekgpress.com [email protected]
RV Injury
Generally accepted "clues" for RV injury are ST segment elevation greater in III than in II, and ST elevation in V1. Of course, in the setting of POSTERIOR MI, the ST depression in V1 can "cancel out" the elevation caused by RVMI. I have seen many ECGs in patients with RVMI and PWMI where V1 had a "flat" ST, or slightly coved, as it tried to show both the elevation and depression. Of course, right sided leads, such as V3R and V4R, are the gold standard. The are lateral enough to avoid the influence of the posterior wall.
Dawn Altman, Admin
Acute RCA Occlusion - with Infero-Postero STEMI
Highly interesting ECG by Dawn on many levels:
----------------------------------------------
On the most Basic Level - there is sinus rhythm with obvious acute infero-postero-lateral STEMI:
On a More Advanced Level:
On an Even More Advanced Level:
Ken Grauer, MD www.kg-ekgpress.com [email protected]
RV-involvement
Indeed, a nice example of RV-involvement in a proximal occlusion of the right coronary artery. Of course, as Stasinos Theodorou suggests, a right sided ECG, i.e. lead V4R, helps to differentiate whether there is RV-involvement. Another hint here should be the relative big difference in ST-deviation between V1 and V2. Involvement of the posterior wall in a proximal RCA-occlusion would render ST-depression, both in V1 and V2. Here, ST-depression in V1 is relatively masked by ST-elevation of an RV-infarction. This should trigger to consider RV-involvement in a proximal RCA-occlusion.
Dr. Mohamed Boulaksil, MD PhD
Resident in Cardiology
Too Bad We'll Never Know for Sure .... (re RV involvement ... )
I agree with Dr. Boulaksil that the "setting is right" for acute RV involvement (ie, strong suggestion on ECG of acute proximal RCA occlusion). That said - to my eye, the amount of ST depression that we do see in lead V1 is not all that "masked" given relative size of QRS amplitude in V1 and V2. I'd be more inclined to agree with you if the ST-T wave in V1 was more isoelectric - but it's not. So I think it remains open to debate as to whether this ECG does or does not suggest acute RV involvement. Unfortunately - there is no V4R, and no clinical information. Too bad we'll never know for sure ...
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Hi after the works of DR
Hi after the works of DR ANTONIO BAYES DE LUNA do we still consider retaining the name posterior MI
aaa
posterior or lateral?
Good question from aaa! Although AHA have said that they are sticking with the term 'posterior MI' for now, I personally have been impressed by the evidence of Bayes de Luna and others and believe that the characteristic ECG changes of 'posterior' infaction are actually due to lateral wall damage. I suspect that it's just a matter of time before AHA is persuaded by the evidence from MRI and changes its guidance but the current terminology has been in place for decades so it's perhaps understandable that things don't change overnight.
Dave R