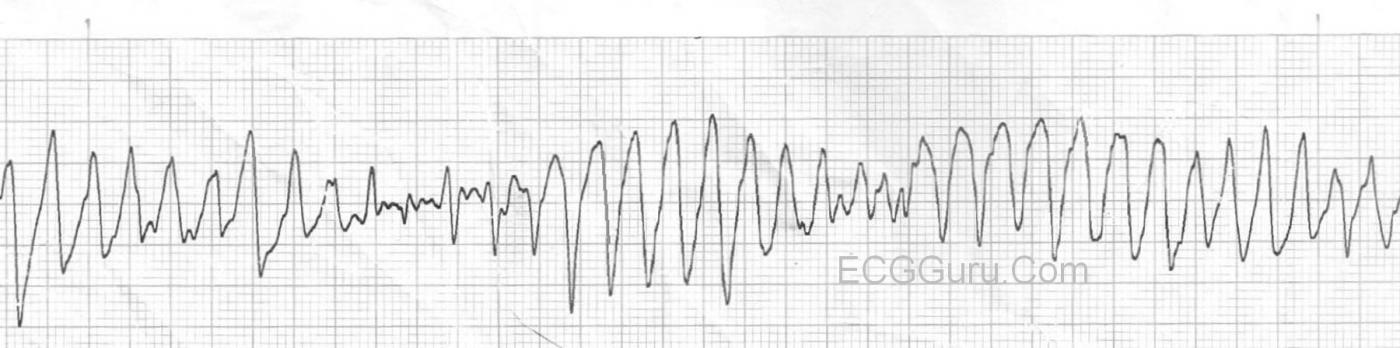
Torsades de pointes, or polymorphic ventricular tachycardia, is a ventricular tachycardia precipitated by and associated with long QT Syndrome. Long QT Syndrome can be congenital or acquired. Torsades is life-threatening, and can be made worse by many drugs, including some of the drugs used to treat VT. The rate is usually 150 - 250 / min. and the appearance is of a wide-complex tachycardia with QRS morphology changes. In some leads, it will appear as if it is "twisting" around the isoelectric line, giving it the French name, Torsades de pointes, a ballet term meaning twisting of the points. For a thorough discussion of Torsades, check this LINK.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Torsades vs Polymorphic VT - The Same But NOT the Same ..
Ken Grauer, MD www.kg-ekgpress.com [email protected]