This series of ECG rhythm strips shows a paroxysmal supraventricular tachycardia successfully treated with adenosine. The patient was complaining of a rapid heart rate and palpitations, but was hemodynamically stable. It is not known whether any parasympathetic stimulation, such as a Valsalva maneuver or carotid sinus massage, was used initially.
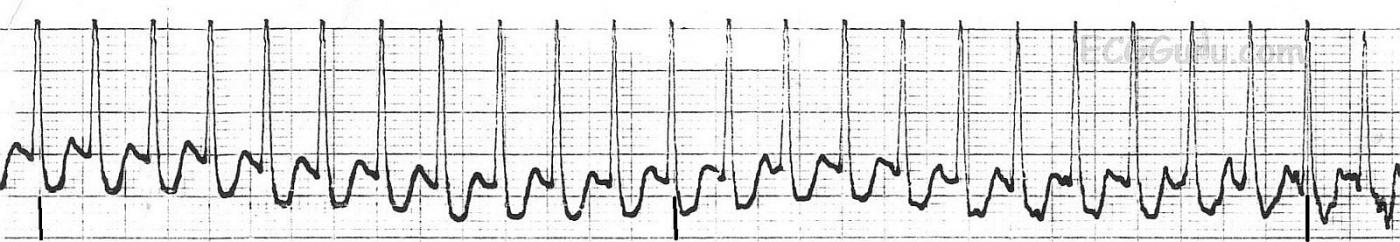
The first rhythm strip shows a PSVT, presumably AV nodal reentrant tachycardia, at a rate of about 215 per minute. (We originally indicated a rate of 240 per minute, but this was a typo). Using the simplist method of determining rate, the six-second method, we see 21, but almost 22, QRS complexes in six seconds. Differential diagnosis would include sinus tachycardia, but this rate is too fast for sinus tach, especially in a resting patient. Also, sinus tach would slow down as the patient is rested or made more comfortable, and this rate did not vary. Also, when confronted with a supraventricular tachycardia, one should also consider atrial flutter and atrial fibrillation. This is somewhat slow for atrial flutter with 1:1 conduction, and that rhythm is much more rare than AVNRT. It is too regular for atrial fibrillation. So, we are left with the probable diagnosis of paroxysmal supraventricular tachycardia. The “paroxysmal” part is presumed since AVNRT has an abrupt onset, and the patient’s symptoms started suddenly.
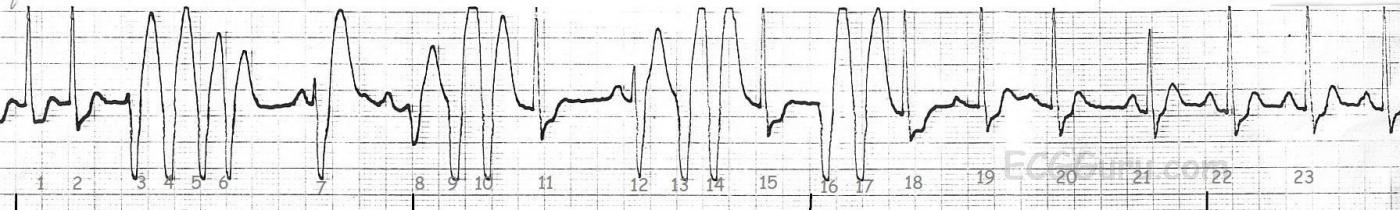
The second rhythm strip shows what happened after adenosine was administered. The patient received first a 6 mg dose, rapid IV push. When that was not effective, he received 12 mg rapid IV push. The rhythm strip is typical of the first minute or so after adenosine administration. Adenosine can cause transient AV blocks, escape rhythms, and ectopic irritability. The half-life of adenosine is only 6 seconds, so the dysrhythmias and uncomfortable symptoms are short-lived. In this strip, we see frequent PVCs and runs of V tach.
An interesting feature of this strip is FUSION BEATS. In ventricular rhythms, the wave of depolarization travels backwards (retrograde conduction). If the ventricular beat is timed just right, it might meet a sinus beat on its way down the conduction system. The two impulses will fuse and the QRS complex will look like a hybrid of the two. Beats 1 & 2 show the PSVT, beats 3, 4, 5, and 6 show a run of V tach. Beat 7 has a sinus P wave, but the morphology closely resembles the PVCs. It is a fusion beat. Beat 8 is a fusion, and 9 and 10 are PVCs. Beat 11 is a sinus capture beat. The P wave is lost in the preceding T wave, but the morphology of the QRS matches the PSVT, indicating normal conduction through the ventricles. After two more PVCs, the patient has sinus beats and a PAC (Beat 20), then settles into sinus rhythm at a rate of about 100/min. Fusion beats prove the existence of a ventricular rhythm, as two sinus or atrial impulses cannot fuse.
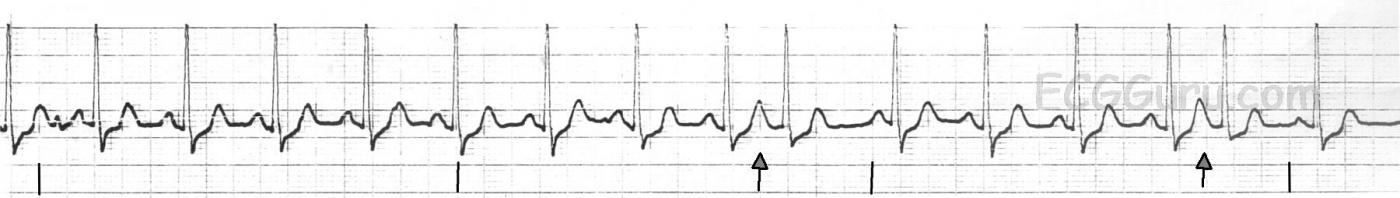
The third strip shows normal sinus rhythm at a rate of about 95 / min with two PACs (arrows). The patient had had quite an exciting time in the emergency department, and his adrenalin caused a fast rate. It appropriately slowed down over the next 15 minutes.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
AVNRT - Adenosine-induced NSVT prior to Conversion
Ken Grauer, MD www.kg-ekgpress.com [email protected]