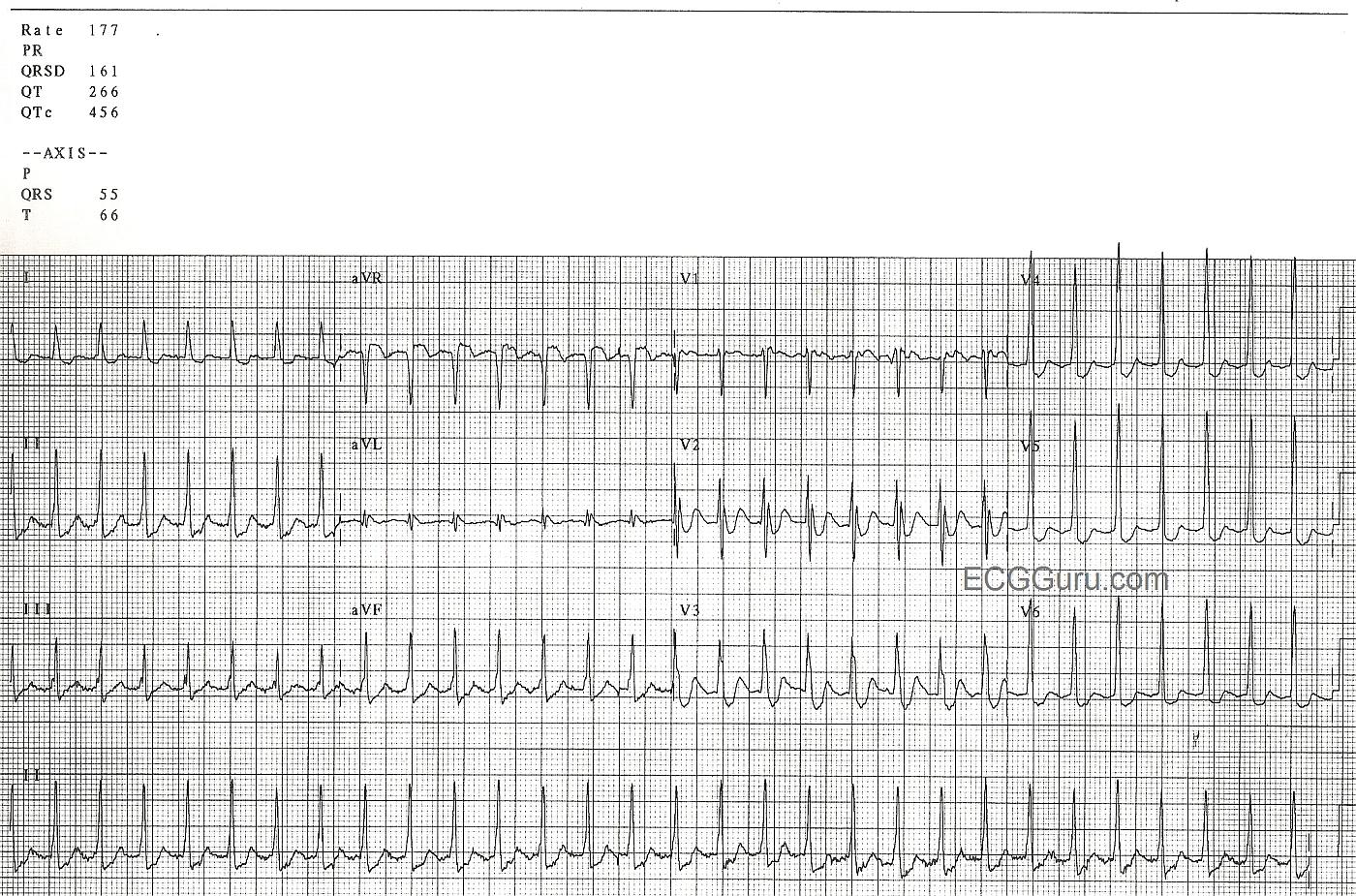
This ECG is from a man in his 60's who is experiencing chest discomfort and palpitations. The onset of the rapid heart rate and the symptoms was sudden, while he was at rest. The rate did not slow when he was placed on oxygen, given IV fluids, and rested further. The rate is 177 / min.
The rhythm is AV nodal reentry tachycardia (AVNRT), which is one of the rhythms that falls into the category of paroxysmal supraventricular tachycardia (PSVT).We can see signs of retrograde P waves in some leads (II, III, aVF, V1). AVNRT is caused by a reentry circuit in the AV node.
Some instructors teach students that sinus tach is approximately 100-150 per minute, and atrial tach is usually 150-250 per minute. If students only learn about differentiating these two rhythms by the rate difference, it will cause later problems. Of course, there is actually an overlap in rates between the two rhythms. For example, a febrile, dehydrated infant could easily reach this rate and be in sinus rhythm. A young, healthy person on a treadmill could, too. Clues to the ectopic origin of this rhythm are: sudden onset (unfortunately, not witnessed here), regular rhythm with unwaivering rate, and the patient's situation (symptoms while at rest, no obvious reason for sinus tach). Of course, we need to teach to the level of our students' abilities. Consider whether they just memorizing rhythms criteria now, or are they learning about re-entry?
There are many different mechanisms of supraventricular tachycardia, and they differ on an electrophysiologic basis. Depending upon the level of your students, you will have to decide how much detail to teach. There are many resources on this site, including the ECG Archives, Ask the Expert, Jason's Blog, and Favorite Sites that will help you if you want to go into more detail. For many health care providers, the entire category of "PSVT" is treated the same initially, and there is no need to differentiate the types of PSVT.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
A Regular SVT without clear sign of Sinus P Waves ...
Ken Grauer, MD www.kg-ekgpress.com [email protected]