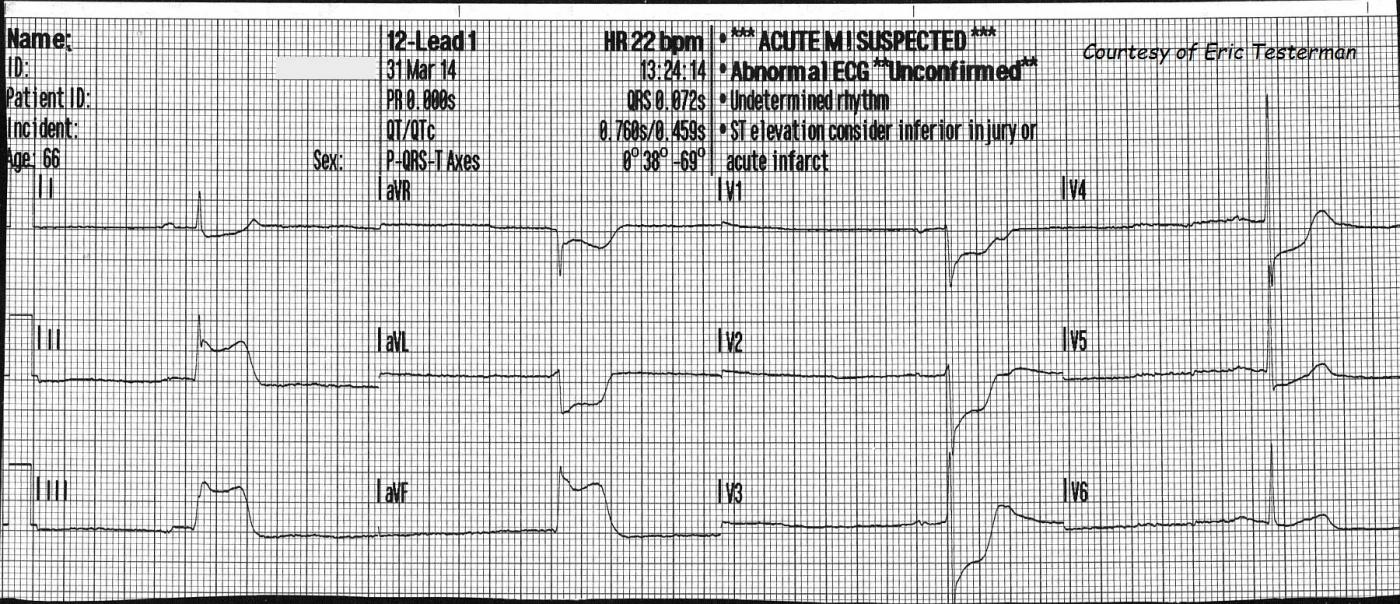
Another great ECG donated by Paramedic Eric Testerman. This ECG is from a 66 year old man who was complaining of feeling dizzy, weak, and of having "minor" chest pain. He was extremely pale/ashen, had moderate cyanosis, and was very clammy and diaphoretic. His initial heart rate was about 20 bpm. His initial BP was 131/113 then, just before arrival at the hospital was 127/85. His HR increased to about 50 bpm (not shown). He was given 400 ml I.V. fluid, 324 gr of aspirin, and oxygen. Transcutaneous defibrillator/pacemaker pads were applied.
At the hospital, he was successfully treated with angioplasty for a 100% occlusion of the right coronary artery. The time from beginning of treatment to reperfusion of the artery was 47 minutes, which is very good!
This is a "classic" inferior wall M.I., with ST elevation in leads II, III, and aVF. There are reciprocal ST depressions in I and aVL. There are also ST depressions in V1 through V5. This is generally considered to represent reciprocal ST changes in the posterior and lateral walls.There is a quite severe bradycardia, and the patient's skin showed signs of poor perfusion. Amazingly, the patient's BP stayed adequate during transport. Bradycardia is common in inferior wall M.I. due to ischemic effects on the SA node and vagus nerve (sinus bradycardia) and the AV node (heart block). In this case, the rhythm is sinus bradycardia. The heart rate is in the 20's, and the PR interval is around .20 - .22 seconds.
This patient's unstable condition and close proximity to the hospital prevented the EMS crew from getting a second ECG, but when there is time, a repeat ECG with a V4R lead can be helpful in deciding how much I.V. fluid is safe to give. This patient's heart rate improved spontaneously during transport, but had it not, the transcutaneous pacemaker could have been used. In some protocols, a trial of Atropine is advised. In others, treatment goes straight to the pacemaker or to I.V. epinephrine. During the angioplasty, a transvenous pacemaker is often inserted into the right ventricle to support the patient's rate if necessary.
This patient was fortunate to be in an area with advanced paramedics and an interventional cath lab close by. It is notable that he never developed pathological Q waves, and hopefully had an uneventful recovery.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute Infero-Postero MI with Marked Bradycardia
Ken Grauer, MD www.kg-ekgpress.com [email protected]