This patient was seen by his primary care provider (PCP) on an outpatient basis. The PCP decided to send her patient over to me to perform a routine ECG and establish a baseline, hince the computer's statement below of "No previous ECGs available". I printed out the above 12-lead ECG and became slightly concerned with the rhythm I was seeing. Consequently, I also recorded six full pages of continuous rhythm (not shown here). I don’t ordinarily resort to doing this except on those rare, special occasions where a longer view helps to elucidate if there is a repeating pattern as well as determining if subtle waveforms are marching our regularly. Not wanting to be an alarmist or cause the patient any undue anxiety, I calmly explained that I wanted to show his ECG to his provider in person. Despite the patient’s assertion that he felt just fine, I immediately accompanied him back over to his clinic so his PCP could further evaluate him. The patient had no known history of irregular or slow heart rhythm.
Patient’s clinical data: 83-year-old white man with history of benign hypertension and diabetes. Medications include glyburide, hydrochlorothiazide, lisinopril, metformin, aspirin, and diltiazem. Around the time this ECG was recorded the patient's blood pressure was hypotensive at 108/37 in the left arm while sitting upright in a chair. The patient had no complaints and was asymptomatic.
Computer’s interpretation:
Atrial fibrillation Slow ventricular response with competing junctional pacemaker
Abnormal ECG
No previous ECGs available
Questions: DO YOU AGREE WITH THE COMPUTER? Is this atrial fibrillation with slow ventricular response and a competing junctional pacemaker? If so, what drug toxicity can cause AV dissociation between atrial fibrillation and a coexisting junctional pacemaker? Is there any form of AV block? If so, is this due to complete AV block? Does this patient have sick sinus syndrome secondary to his advanced age and require implantation of a permanent pacemaker? Does the word “iatrogenic” have any place in this scenario?
Difficulty rating: * * * * (i.e., intermediate to advanced)
-
- jer5150's blog
- Log in or register to post comments
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
heart stopping strip
Nice and heart stopping strip Jason. Let me try...
I think there is a "hump"/distortion on the first T wave which could be a P wave. This is followed 1600 ms later with another P wave that shows to be conducted. The 3rd P wave could be hidden from view on the 4th QRS complex. The 5th P wave is distorting the T wvave of the 5th QRST complex which can be observed by comparing T wave shapes in V2 (5th vs 6th complexes).The 6th P wave can be seen before 7th QRS complex (condcuted normally).The 7th P wave seemed to distort the last QRS complex (comparing complexes 7 and 8 in V1). So this is sinus baradycardia (about 37)
QRS conplexes 1,2, 4,5, 6 and 7 are junctional escapes at a rate of 40's (1400 ms).
So this could be profound sinus bradycardia with junctional escape.
If there is no other drug that this patient is taking aside from diltiazem then this couild be the culprit. A liver panel might warranted (hepatic metabolism of diltiazem) and review of the dose. Take off/substitute the drug and observe the clinical response of the patient. Maybe reserve PPM later.
I think this is level 4 or 5 (for me).
RHY
Sinus 1st degree, JER and P wave in some st segments.
INTERPRETATION
Comments:
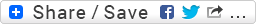
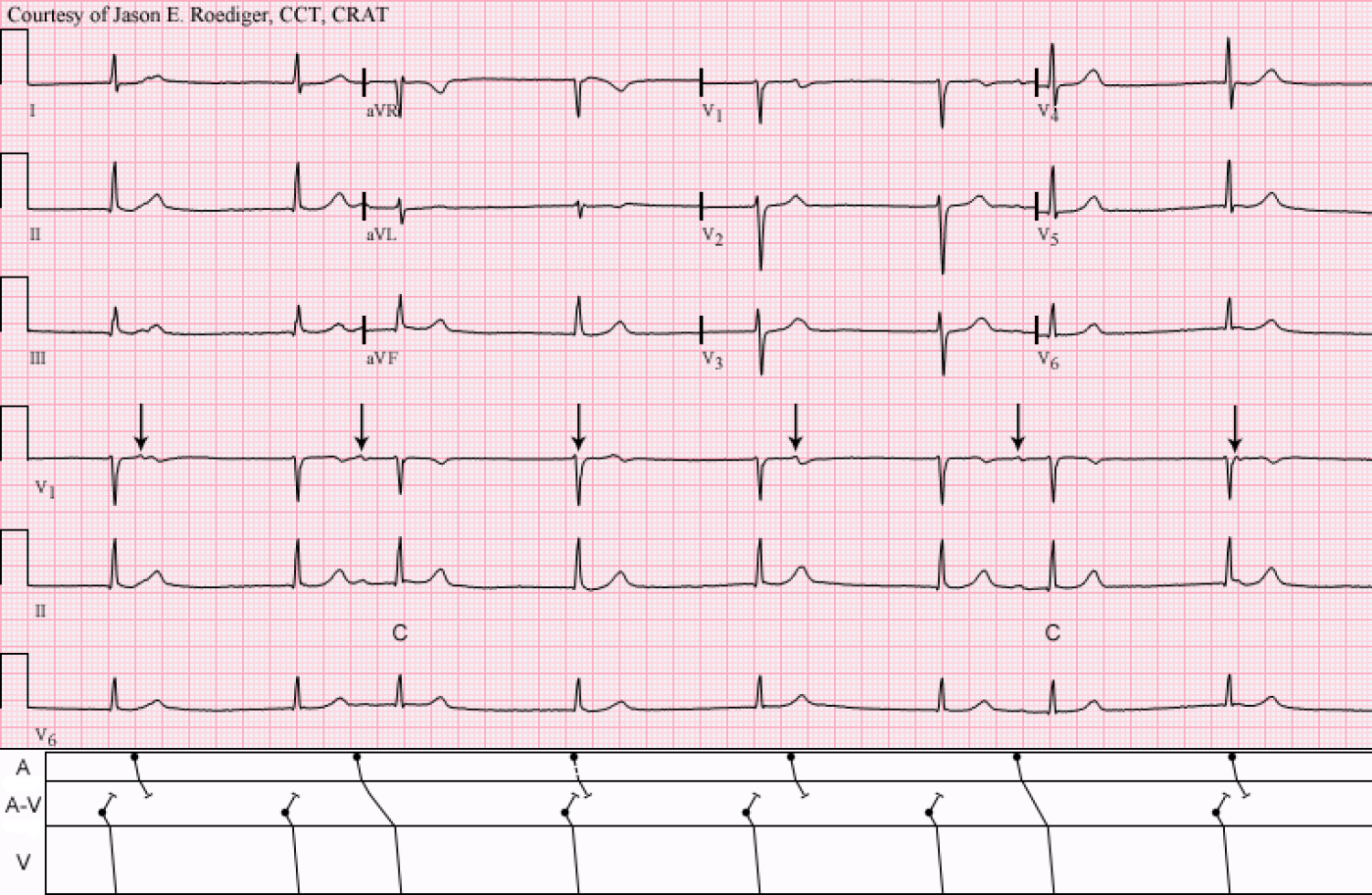
It was determined that this patient had diltiazem intoxication/poisoning which was markedly slowing down his sinus rate. Note the sinus P-waves marching out regularly from left to right; see arrows (↓). The patient’s PCP discontinued his diltiazem and, as an alternative medication, she started him on amlodipine 2.5 mg PO daily. She also had him report back for a follow-up appointment 13 days later at which time his ECG now showed normal sinus rhythm with so-called “first-degree” A-V block. Therefore no indication for a PPM.
It’s paramount to remember that the only primary disturbance here is the sinus bradycardia. The resulting junctional escape rhythm, A-V dissociation, and ventricular captures (C) are all secondary to the slow sinus rate. Merely withdrawing his diltiazem magically “cured” everything by allowing the sinus node to accelerate back up to a normal rate. Healthcare providers have a tendency to get overwhelmed by all of the overlapping features and as a result the rhythm is often misinterpreted and consequently the patient is mismanaged. This PCP took the right approach and did not overreact by ordering needless and expensive testing like an electrophysiology study. She correctly deduced that the dilt was the most likely culprit and removed the offending drug.
INTERPRETATION: (Top tracing)
1.) Sinus bradycardia (rate about 37/min) with resulting . . .
2.) . . . junctional escape rhythm at a slightly faster rate of about 44/min producing . . .
3.) . . . A-V dissociation.
4.) Two ventricular captures (3rd and 7th beats) with prolonged P-R intervals (0.29s and 0.24s
respectively) displaying . . .
5.) . . . R-P/P-R reciprocity (see laddergram).
INTERPRETATION: (Bottom tracing)
1.) Sinus rhythm (rate about 73/min) with . . .
2.) . . . “first-degree” A-V block (P-R = 0.28s)
References / Sources:
1.) http://en.ecgpedia.org/wiki/Answer_-_Case_of_the_month_%28Feb_2012%29
Jason E. Roediger - Certified Cardiographic Technician (CCT)
[email protected]