The Patient: A 75-yr-old man called Emergency Services because of chest pain and shortness of breath. He had just returned from a 15-mile bicycle ride, during which he had to stop several times to catch his breath, not normal for him. He was so diaphoretic, they were not able to get a good 12-lead ECG. While the paramedics were assessing him and preparing for transport, he went into ventricular fibrillation. He was defibrillated at 360 joules within seconds of onset, and converted to sinus rhythm with pulses.
The ECGs:
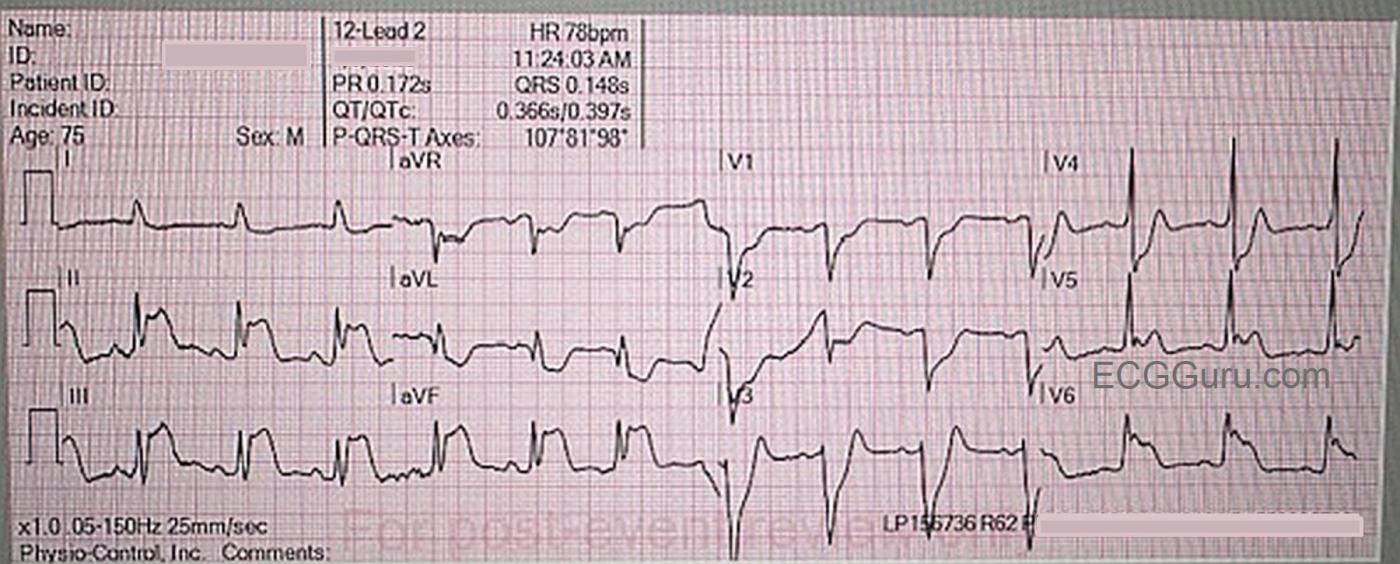
11:24 am: This ECG is obtained after defibrillation, and there is return of spontaneous circulation (ROSC). The rhythm is sinus at 78 bpm. The QRS is slightly wider than normal at .12 seconds. (It is my opinion that the ECG machine read the QRS wider because of the J point and ST changes.) Other intervals and frontal plane axis are within normal limits. R wave progression is normal.
There is marked ST elevation in Leads II, III, & aVF, with reciprocal ST depression in Leads I, aVR, & aVL. (inferior wall transmural injury). There is ST elevation in V5 and V6 (low lateral transmural injury), and ST depression in V1 through V4 (posterior-lateral transmural injury with reciprocal changes in these leads.)
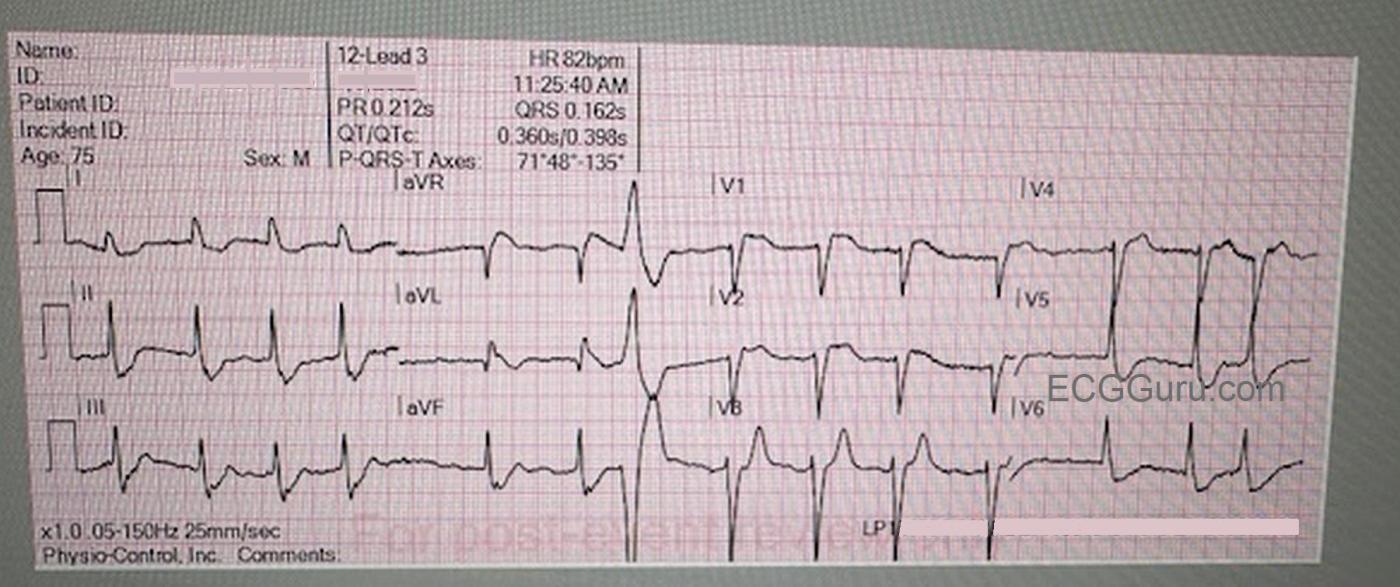
11:25 am: The rhythm has changed. There are no clear P waves, and the rhythm is irregularly-irregular. This is atrial fibrillation, with one PVC. Not only that, the ST changes are completely different. The inferior wall now has ST depression, with reciprocal elevation in aVL. There is now ST elevation in right sided chest leads V1 and V2, as well as ST depression in V5 and V6. The ST changes of acute M.I. can vary as the supply-demand ratio shifts. As demand increases, or supply decreases, the ST segments will elevate, indicating transmural ischemia/injury. If demand decreases or supply increases (arterial dilation, increased cardiac output, etc.), the ST elevation will disappear, and ST depression will represent ischemia that is not transmural. BEWARE: Unless this occurs after catheterization and angioplasty or pharmaceutical thrombolytics, the obstruction is still there, and will probably increase again.
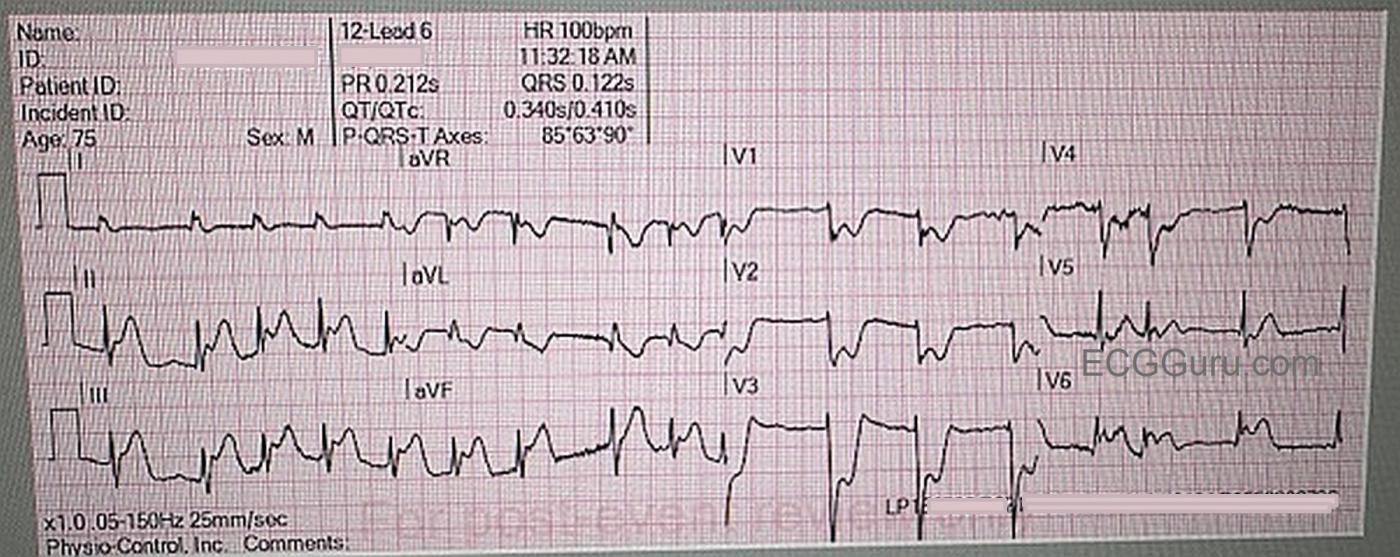
11:32 am: The rhythm is still atrial fibrillation, with a tendency to be fast at times. The ST elevation is back in the inferior and low lateral walls. There are “appropriate” reciprocal changes in the limb leads I, aVL, and aVR. V1 through V4 have ST depression reflecting the ST elevation that is on the back of the heart.
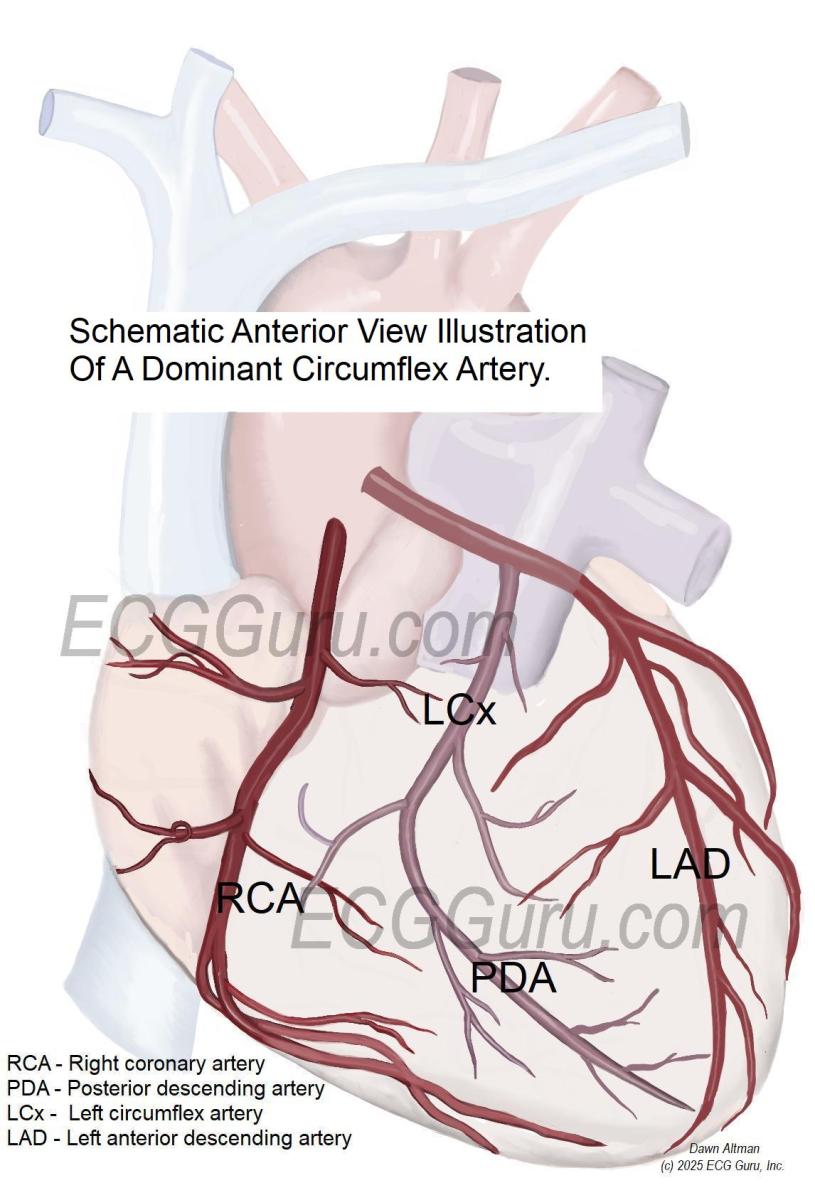
Outcome: The patient was taken to the cath lab on admission to the hospital. He was found to have a non-dominant right coronary artery (RCA), which was patent. His dominant left circumflex artery (LCx) was 100% occluded. The posterior descending artery (PDA), which supplies the inferior and posterior walls, arises from the right coronary artery in 70-80% of the population. The PDA arises from the LCx in 8-10% of the population. In 10-20% of people, the PDA is supplied by both the RCA and the LCx.
This patient had a successful recovery, and was discharged from the cardiac ICU after two days, with a Cerebral Performance Category of 1 (CPC-1) – no neurologic deficits. This is a great case to illustrate two important points: 1) During an acute occlusive event, the ECG can change minute-to-minute. It is important to obtain serial ECGs on anyone having chest pain or other symptoms suggestive of M.I. Remember, IF THE PATIENT IS SWEATING IN A COOL ENVIRONMENT, YOU SHOULD BE, TOO. 2) Early, prompt treatment by personnel capable of defibrillation and resuscitation, along with access to an interventional cath lab, makes a huge difference in survivability in an occlusive M.I. (OMI). There is great disparity between geographical locations regarding the availability of defibrillators (including Automatic External Defibrillators), people trained to use them, quick response and transport times, and nearby hospitals that have comprehensive cardiac services. This patient was fortunate to arrest in an area with very advanced EMS agencies and nearby hospitals with a full range of cardiac services
Our thanks to Ashley Terrana, Paramedic, for contributing this case.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
A Lucky Patient & 3 ECGs with a Fascinating LOT of Questions!
Today's patient is LUCKY to be alive. Had he not been in as good physical shape (for his 75 years) as he was — he probably would not have been able to complete his 15-mile bike ride — and therefore be in position to summon EMS — and be promply defibrillated. Instead, had his arrest occurred during (insead of after) his bike ride — he would not have survived.
For clarity — I have reproduced today's 3 serial tracings in the figure below. Hard to believe that LESS than 2 minutes separate ECG #1 and ECG #2 — with less than 7 minutes separating ECG #2 and ECG #3. These serial tracings highlight a number of important points.
As per Dawn — Computer ECG interpretations need to be overread. Although the QRS complex in lead I of ECG #1 "looks" a little bit wide — the actual QRS duration is probably no more than 0.10 second (whereas the computer thinks the QRS is well over 0.14 second on each of the first 2 ECGs). There is no bundle branch block on these tracings.
I woud not have necessarily guessed a LCx (Left CircumfleX) "culprit" on the basis of ECG #1. Clearly, there is dramatic ST elevation in lead V6 (with terminal QRS distortion in the form of a markedly elevation J-point without any S wave) — but there is even more ST elevation in leads II, III and aVF — with maximal ST elevation in lead III, and marked reciprocal ST depression in lead aVL (but not in lead I) — all of which points more to an RCA (Right Coronary Artery) "culprit". Marked ST depression in leads V2,V3,V4 (much more than in lead V1) are diagnostic of associated posterior MI. As per Dawn — the result is dramatic ST-T wave deviation from an extensive acute infero-postero-lateral STEMI ( = further attestation about the power of prompt defibrillation that saved this patient's life!).
The fascinating finding about these serial ECGs — is that less than 2 minutes later, the patient is in AFib — with almost complete REVERSAL of his dramatic ST-T wave deviations! Were I to be shown ECG #2 without seeing ECG #1 (and told this patient had just been defibrillated) — I would have interpreted ECG #2 as either showing diffuse subendocardial ischemia (ie, ST depression in 7 leads, with ST elevation in aVR >V1) — and/or as suggesting "Precordial Swirl" predictive of a proximal LAD occlusion (ie, diffuse ST depression — except for ST elevation in aVR, aVL and V1,V2).
Instead — knowing from ECG #1 that this patient had extensive posterior wall involvement — the only way that I know how to explain the dramatic switch from ECG #1 — to ECG #2 (in less than 2 minutes) — with reversal of these changes in ECG #2 to an almost "repeat picture" of ECG #1 in ECG #3 — is that there has been spontaneous reperfusion of the "culprit" LCx artery (with the greatly increased T wave amplitude in lead V3 of ECG #2 strongly supporting posterior reperfusion — as well as virtual resolution of ST elevation elsewhere, with now ST elevation insead of depression in lead aVR). This "spontaneous" reperfusion however only lasts 7 minutes, with reocclusion of the LCx in ECG #3.
MY EXPLANATION for the fascinating above Findings = This patient has to have some complex pattern of multivessel disease, probably ongoing over years — with an equally complex pattern of collateral flow that "flipped" for a few minutes with brief spontaneous reperfusion that prompted the dramatic ST-T wave reversals that we see.
This patient is truly lucky to be alive!
NOTE — The purpose of the schematic coronary artery figure shown above is simply to illustrate the theoretical vascular distribution of a patient with a dominant LCx that solely supplies the PDA (without contribution from the RCA). The duller red coloring represents vessels "behind" our visual perspective. The specific lesions found on this patient's cardiac catheterization are not shown. (And we are not told about the multivessel interventions on PCI — if not CABG that this patient received as treatment.)
Ken Grauer, MD www.kg-ekgpress.com [email protected]