The Patient: 67-year-old man complaining of chest pain radiating to his jaw, 10/10. He is short of breath and diaphoretic. We do not know his BP, just that it was low. The patient states “no past medical history – never hospitalized”. He thought himself to be very healthy. He was given aspirin 325 mg and transported to a full-service cardiac hospital as a “cardiac alert”.
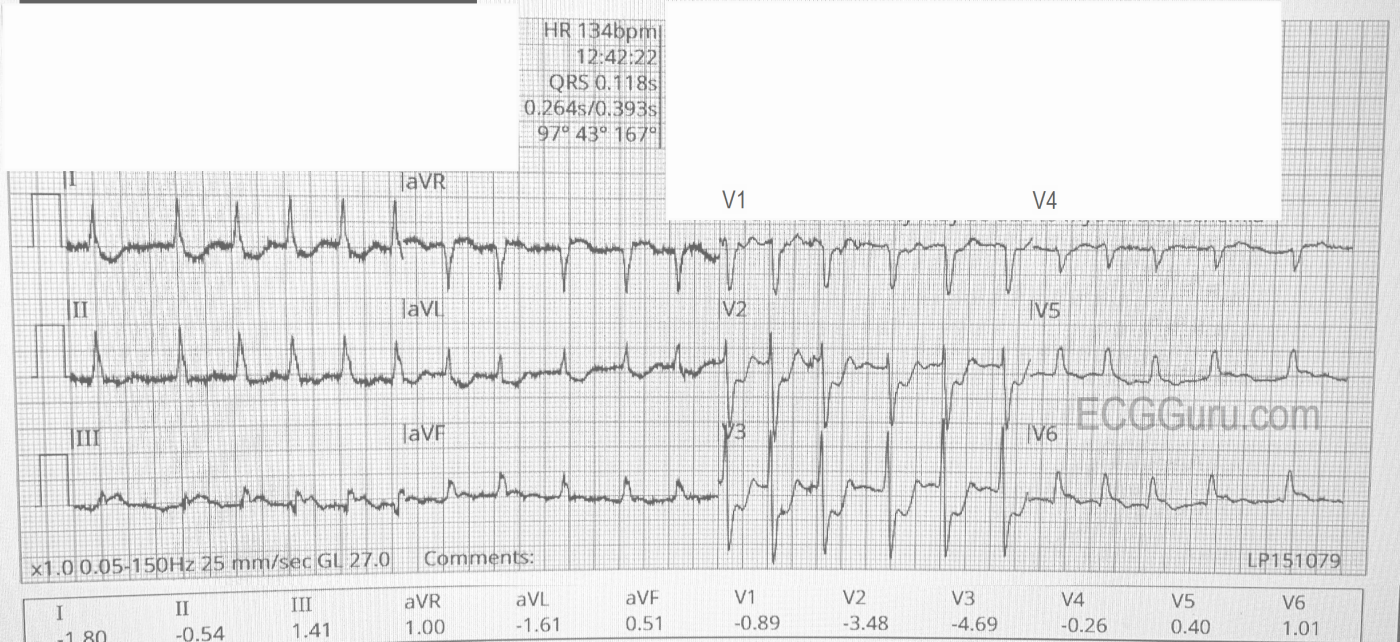
The ECG (from EMS):
The rhythm is atrial fibrillation with a rapid ventricular response (about 134/min.). The QRS width is .118 seconds (118 ms). The frontal plane axis is slightly to the left, but WNL. The R wave progression mostly normal, but V4 is incongruous. V2 and V3 have a tall R wave, possibly representing a pathological Q on the posterior side. There are ST CHANGES in every lead. ST elevation is noted in III, aVF, aVR, V5 and V6, representing ischemia in the inferior wall. There is ST depression in all other leads, indicating widespread subendocardial ischemia and/or acute reciprocal depression. Interesting that Lead II would normally be elevated when III and aVF are, but aVR is elevated, causing reciprocal ST depression in Lead II. So, Lead II looks almost normal.
The pattern of ST elevation in aVR with widespread ST depression can indicate:
1) Proximal occlusion of LAD or significant stenosis of Left Main artery.
2) Severe triple vessel disease
3) Any condition that results in cardiogenic shock
Often, there is also STE in V1 in this situation, but V1 – V3 show signs of posterior MI, with definite ST depression and tall R waves in V2 and V3.
It is obvious that this patient’s condition is extremely dire, and he would earn a trip to the cath lab on symptoms alone in most places. An inexperienced observer might not recognize the importance of the ST elevations, since they are not large, but the pattern of elevation and the widespread ST depression is very alarming.
The Emergency Department: The patient was prepared for transport to the cardiac cath lab, but suffered a storm of ventricular tachycardia and ventricular fibrillation. He was defibrillated multiple times and intubated. He was given magnesium sulfate, amiodarone, esmolol, and bivalirudin.
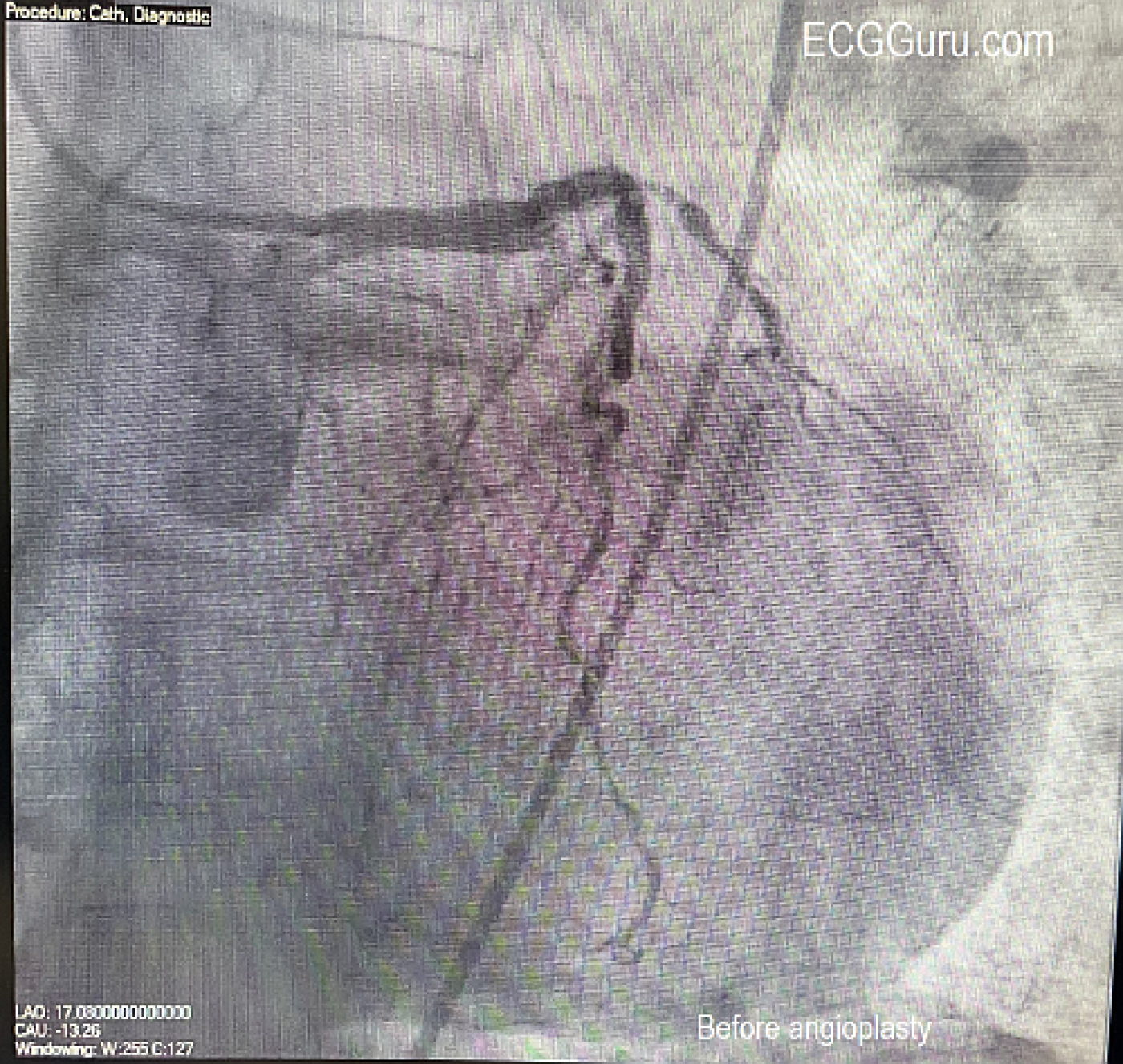
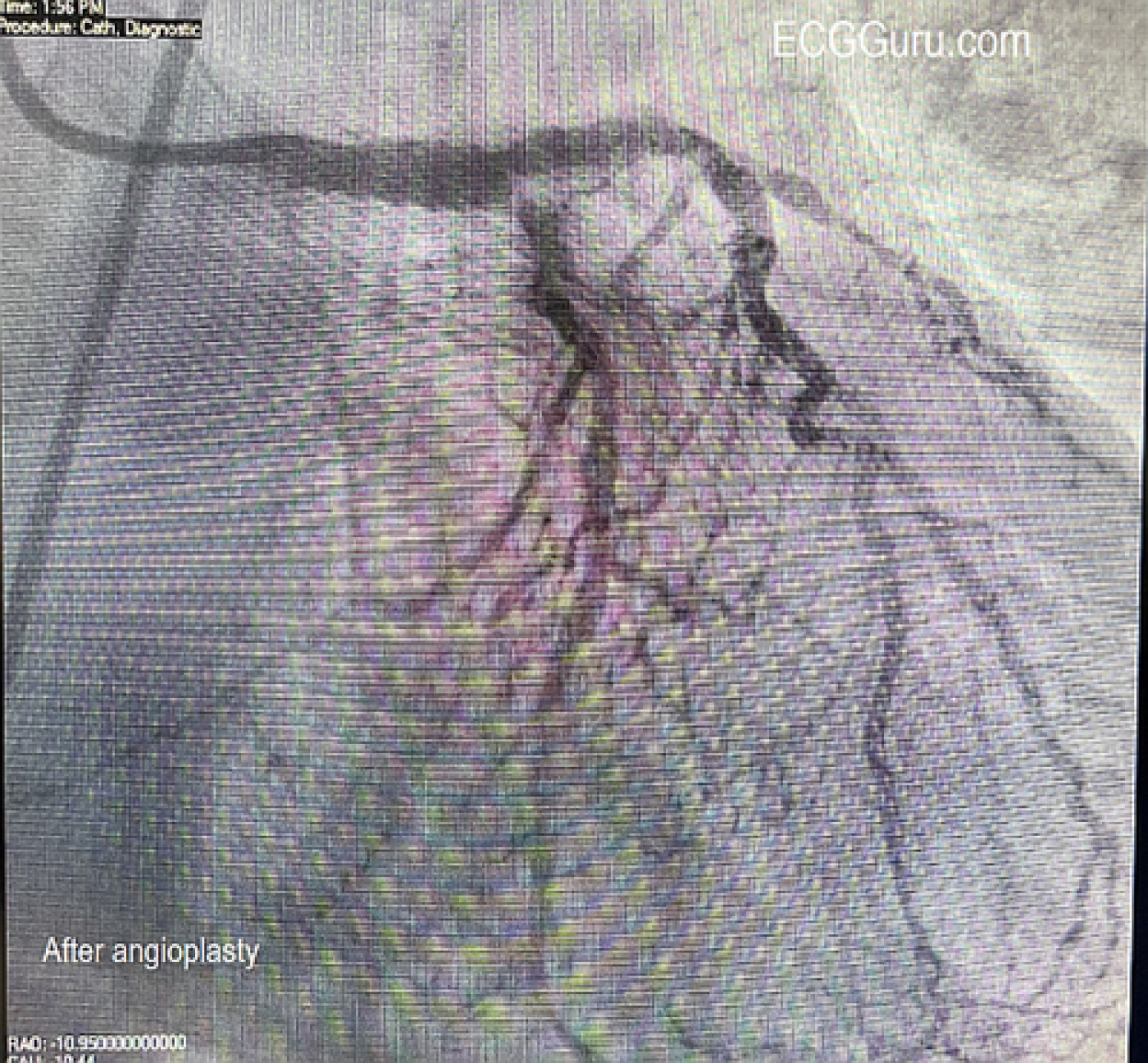
The Cath Lab: In the cath lab, the circumflex artery was found to be totally occluded. When a wire was introduced, circulation opened up, revealing an extensive collateral system from the circumflex to the area usually supplied by the RCA (inferior/posterior wall). The right coronary artery (RCA) was found to have chronic total occlusion (CTO), confirmed by the presence of the collateral system from the circumflex. The arteries show extensive disease. The patient was stabilized with an Impella (mini ventricular pump) placed due to cardiogenic shock. The ECG shows how extensive the damage can be when coronary circulation is relying on one coronary artery system (the left) to supply the entire heart. In this case, the LCx was responsible for the inferior, posterior, and lateral walls, and was occluded. The left anterior descending (LAD) artery was diseased but still patent.
The Outcome: The patient went to surgery for five-vessel coronary artery bypass graft. He did well, and three days later he was awake, alert, having had all central lines, ventilator and ventricular pump removed.
This is a great teaching example emphasizing how important symptoms and presentation are in determining severity of condition. Another good teaching point is that the size of the ST elevation is not necessarily a determination of severity of cardiac damage. Not all OMI patients will present with a nice, neat ECG showing a pattern of one-vessel occlusion with large ST elevations. This is a reminder of the outcomes that are possible in a place that has well-trained EMS and the availability of nearby full-service cardiac hospitals.
Our thanks to Natalie Terrana, RN, EMT-P for contributing this valuable teaching case. She happens to be a friend of the ECG Guru website since our beginnings, and is the one who came up with the name, ECG Guru!
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Positive "Mirror" Test — in a Patient with Cardiogenic Shock
The ECG in today's case tells a story! As per Dawn — there are ST-T wave changes in EVERY lead. Dawn has highlighted these changes in her excellent discussion. I'll focus on a number of selected points.
The presenting rhythm is rapid AFib. If the AFib is new — this presents yet another reason for acute heart failure (cardiogenic shock in today's case) — as there is loss of the atrial "kick" (which in many such patients is critical to cardiac output) — plus the rapid rate of new AFib disproportionately reduces the period of diastole, which accounts for most ventricular filling.
One might be surprised at the lack of marked ST elevation in this patient with cardiogenic shock. But the principal "culprit" artery is the LCx (Left Circumflex Artery) — occlusion of which in today's case produces acute infero-POSTERO-lateral MI. And the posterior wall of the LV is not directly viewed on the standard 12-lead ECG. Although recommendations are often made to "obtain posterior leads V7,V8,V9" when looking for posterior MI — it is much FASTER and EASIER to familiarize yourself with the "Mirror Test". Acute posterior MI produces maximal ST depression in leads V2,V3 and/or V4 — with this ST depression being the "mirror image" of the ST elevation that one would see in posterior leads V7,V8,V9. More than that — the relative amount of ST depression that you virtually always see in these anterior leads is MORE than the amount of ST elevation you'll see in the posterior leads for the simple reason that ST elevation amplitude is attenuated by the thick musculature of back muscles. In more than 4 decades of comparing the mirror test with posterior lead findings — I do not believe I have EVER seen a case of an acute posterior MI in which posterior leads told me something that was not instantly obvious to me from looking at leads V2,V3,V4 in the standard ECG (Looking at the mirror image insert — Isn't acute posterior MI obvious?)
ST elevation in leads III, and especially aVF — as well as in leads V5,V6 is subtle-but-definitely present (Focus on the coved SHAPE of the ST segments in these leads). Putting this together — an acute inf-post-lat MI in which the relative amount of ST segment displacement is clearly greatest in leads V2,V3 localizes the acute occlusion to the LCx.
The clue to underlying multi-vessel disease is the additional marked flat ST depression in leads I and aVL, in association with ST elevation in lead aVR. So the reason we do not see ST depression in the 3rd inferior lead ( = lead II) — is because the ST elevation that inferior MI would normally produce is attenuated by the ST depression that we would otherwise see in lead II from DSI (Diffuse Subendocardial Ischemia).
To emphasize that the ECG picture can be confusing when there is multivessel disease — rapid AFib (in which the fast rate by itself may produce diffuse ST depression) — and an acute MI in a patient with multivessel disease and the often resultant unpredictable patterns of collateralization. BOTTOM LINE — I immediately suspect MULTI-vessel disease whenever I see acute changes with ST-T wave abnormalities in virtually every lead that are not completely "explainable" (ie, Figuring out why we don't also see ST elevation in lead II).
Fortunately in today's case — excellent care resulted in prompt decision-making leading to 5-vessel CABG with the patient doing well despite his presentation in cardiogenic shock. A GREAT success story with many lessons embedded within the initial ECG.
Ken Grauer, MD www.kg-ekgpress.com [email protected]