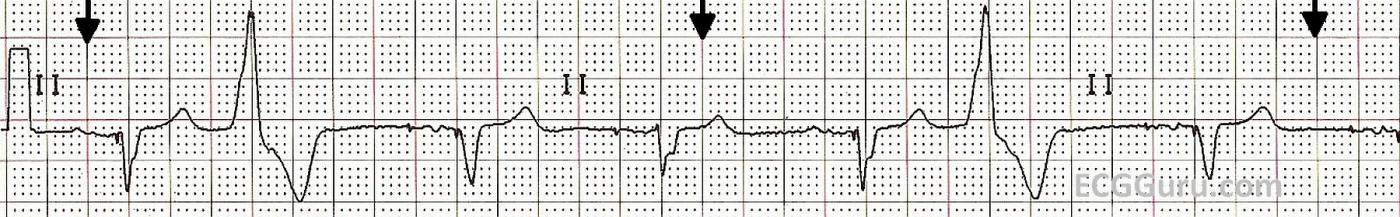
This is a Lead II rhythm strip from a patient with a biventricular pacemaker. The second and sixth beats are PVCs. In this lead, the pacemaker spikes are very difficult to see, but they are present. The pacemaker is operating in a "demand" mode for pacing the atria. Some of the P waves appear to be the patient's own, and some appear to be caused by the pacing stimulus. For example, the first beat appears to have no pacer spike before the P wave, and the second beat does have one (albeit tiny). The morphology of the P waves appears to change, also.
This pacemaker has been programmed to cause a QRS complex after every P, whether the P wave was made by the patient or by the pacemaker. The patient originally had a left bundle branch block, making his QRS complexes very wide, and lowering his cardiac output. The biventricular pacemaker paces both ventricles, synchronizing their depolarization and narrowing the QRS. This improves cardiac output. The physician has programmed this pacemaker to pace the ventricles after every P wave, whether native or paced. The paced QRS happens slightly before the native (wide) QRS would have, giving the patient the benefit of narrow QRS complexes. Biventricular pacemakers have been shown to improve cardiac output in patients with wide complexes.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Sub-optimal programming?
I think there may be a bit more here than is immediately apparent. There is some variation in QRS morphology amongst the paced beats, so I wonder if there is variable fusion. In fact, I suspect that the 4th QRS is nor paced at all. Judging from the 3rd beat, it appears that the programmed paced AV interval is 240ms, yet the next QRS appears to start 200ms after the atrial pacing impulse and there is no sign of a ventricular pacing impulse, suggesting that this may be a conducted beat. Obviously a biventricular pacemaker is only effective if the ventricles are actually paced, so the paced AV interval must be set at a shorter value than the patient’s own conduction time. I wonder if in this case the paced AV interval should be shortened to promote pacing.
Dave R
Thanks, Dave
I wondered myself about the fourth beat. The challenge for me is to present basic strips that teachers of monitor techs and beginner practitioners can use. They are VERY hard to find!!! Sometimes, I ALMOST understand why many teachers use rhythm generators (but not quite). No matter what strip I choose for the basic level, there is always something "advanced" and very interesting about it. Thanks for your insight.
Dawn Altman, Admin
Too short sAV Delay
iTo feel that the sAV delay is too short. Conventionally it should be about 25msec shorter than the pAV Delay to compensate for the 'delayed' sensing of signals.
KinCiong!
Quick question
The biventricular pacemaker is a wonderful thing. It brought a friend of mine's ejection fraction from 20% to nearly 90%. We looked at his EKG on a lifepack 15 just to see it in action and I noticed a few things. Firstly his is a three lead fixed rate A-V sequential pacemaker. The LP15 only picked up on a single ventricular spike and did not "see" the atrial though I am sure it was there. More interestingly was the fact that the QRS was not over .120ms (about .09-.10ms) and the T wave remained upright in lead II, we did not get a chance to play with the 12 lead though I wish we had. When the QRS is so narrow like this, can 12-leads be used in the search for ST elevations despite the fact they are indeed being paced or will there still be artificial ST elevations? ~Neil
Good questions
Hi, Neil,
Yes, cardiac resychronization therapy is a huge breakthrough, especially for those who have wide QRS complexes and heart failure. While the pacemaker itself has many programming options, including "demand" mode, it iif most often programmed to pace at or nearly at 100 %. The idea is to have all paced beats, which are narrow, rather than the patient's "own" beats, which are wide. There is, as you have seen, much better cardiac output with a narrow complex.
Sometimes, spikes are hard to see. But in the case of CRT, the patient usually has an intrinsic sinus rhythm and does not need the pacemaker to pace the atria. This is in contrast to the pacemaker that is being used to treat bradycardias and AV blocks. Most often, the atrial wire will SENSE the patient's P waves and TRIGGER the ventricular wires to produce a QRS complex. The patient keeps his ability to adjust his rate naturally. As Dave Richley mentioned in his comment above, the pacemaker is programmed to have a shorter AV interval (PRI) than the patient's normal one, ensuring that the patient doesn't slip in wide native beats (or fusion), whicMackey be the case in our sample strip.
And, yes, it is not the PACEMAKER that makes it hard to recognize STEMI on the ECG, it is the WIDE QRS. So, if we succeed in narrowing the QRS, we will be better able to detect STEMI.
Glad your friend got such good results!
Dawn Altman, Admin