All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.
Recent blog posts
- New Interactive ECG Quizzes
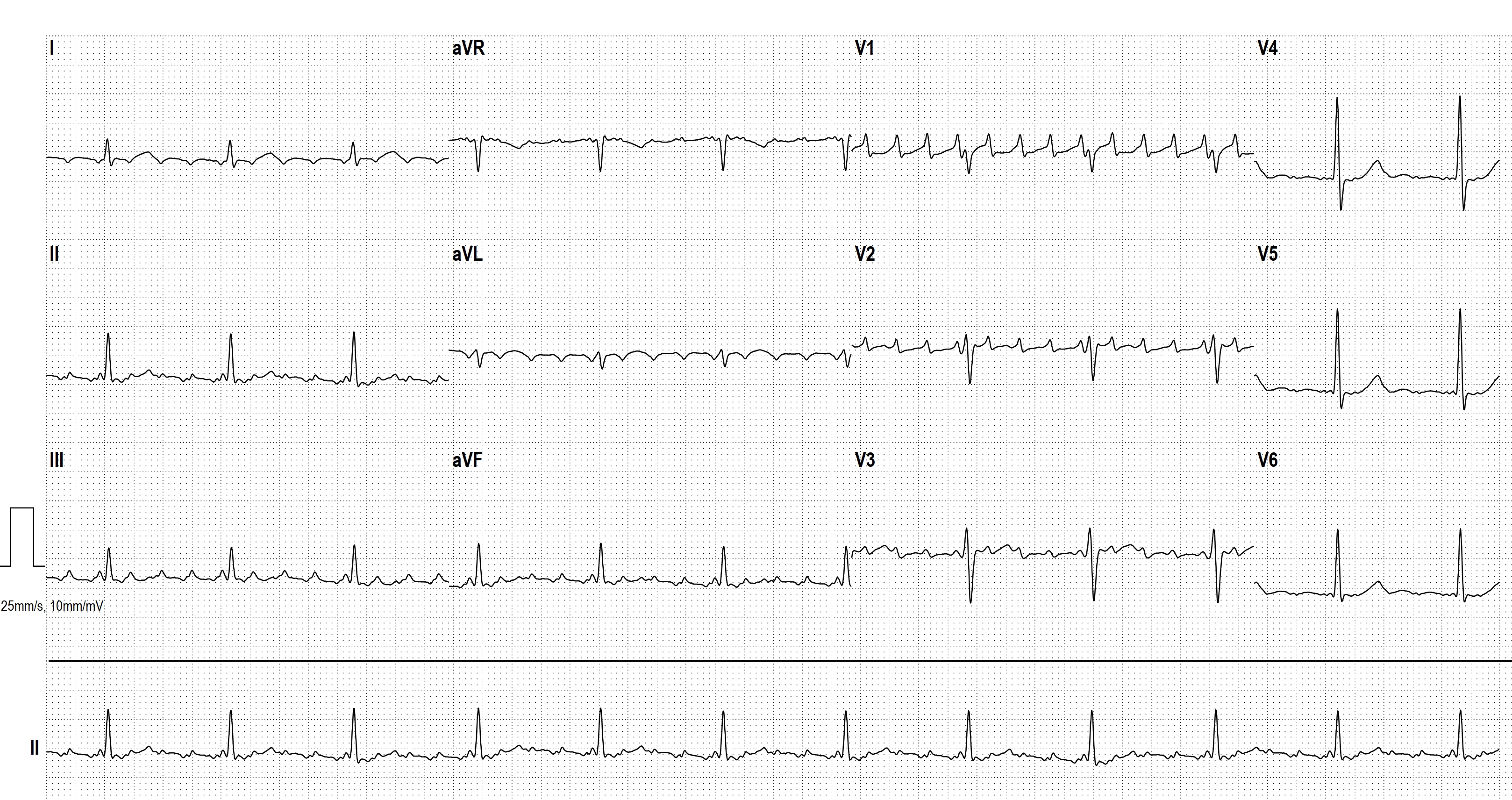
- PACS WITH ABERRANT CONDUCTION
- HOLTER ECG: FAST VT, ATP, ICD SHOCK
- AIVR
- COMPLETE AV BLOCK
- HIGH GRADE AVB
- JUNCTIONAL ESCAPE RHYTM
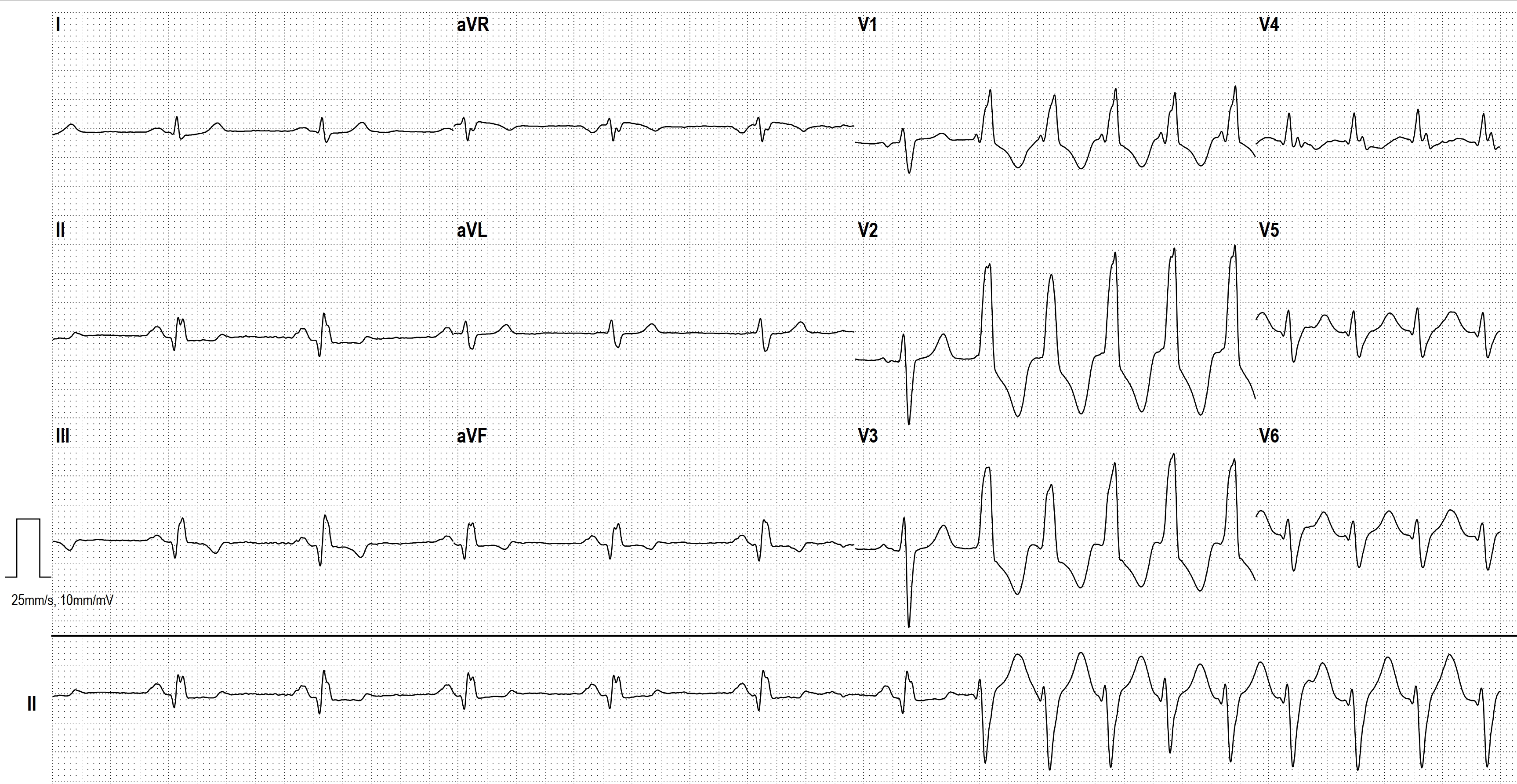
- POLYMORPHIC VT
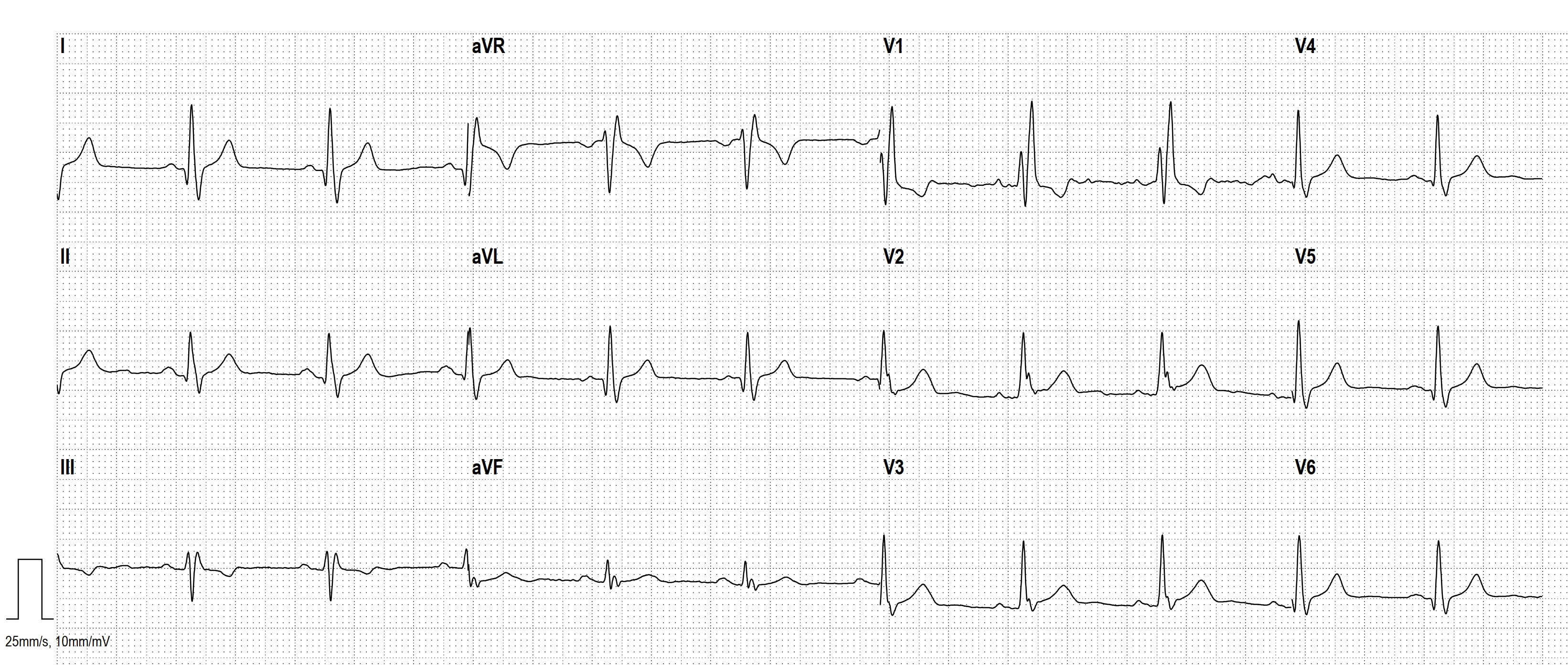
- SGARBOSSA CRITERIA
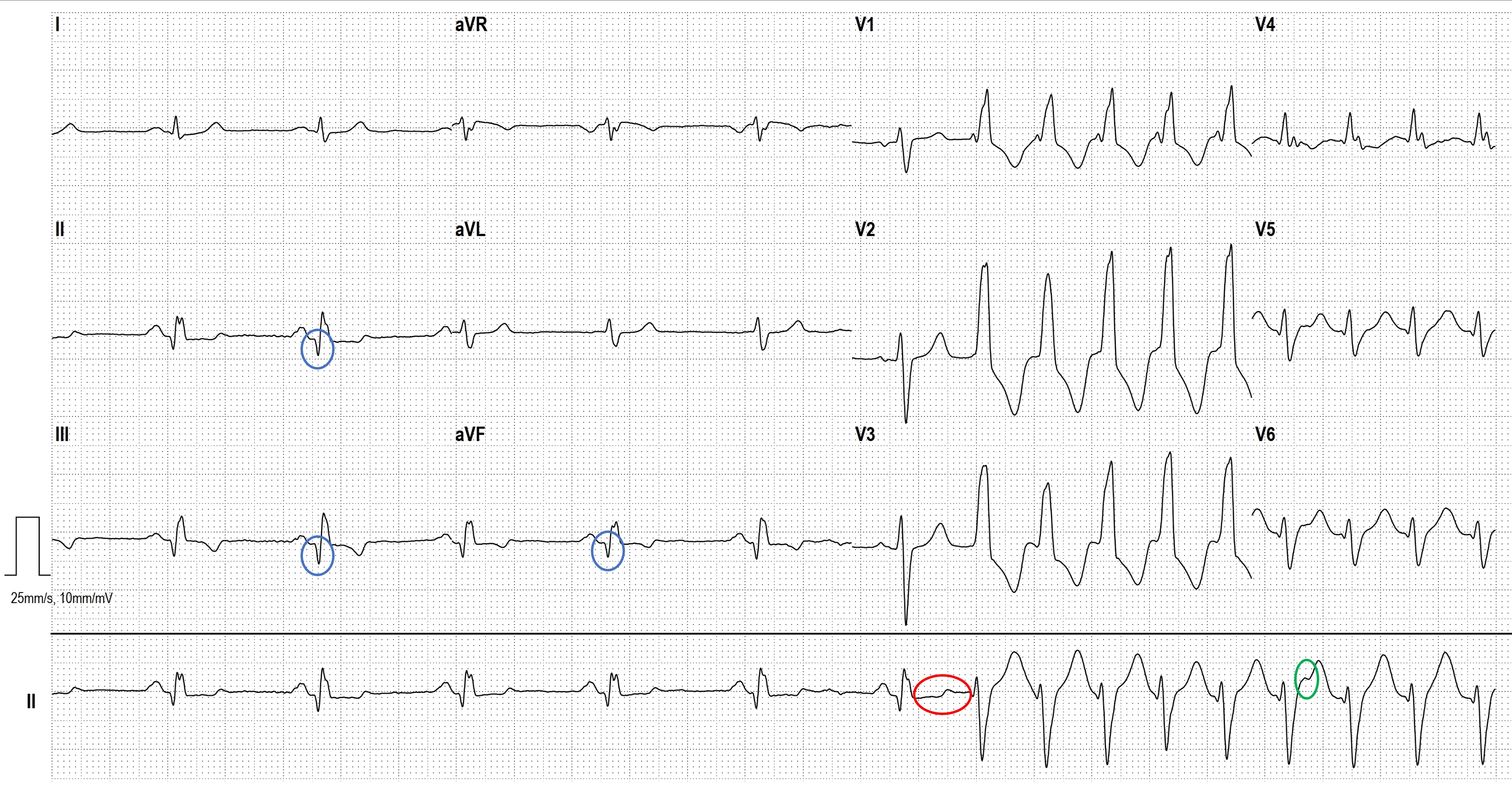
- CONCEALED CONDUCTION
- CONCEALED CONDUCTION AND VENTRICULOPHASIC SINUS ARRHYTHMIA
- PAROXYSMAL ATRIAL FIBRILLATION
- 2nd Degree Sino-atrial Exit Block, Mobitz Type II
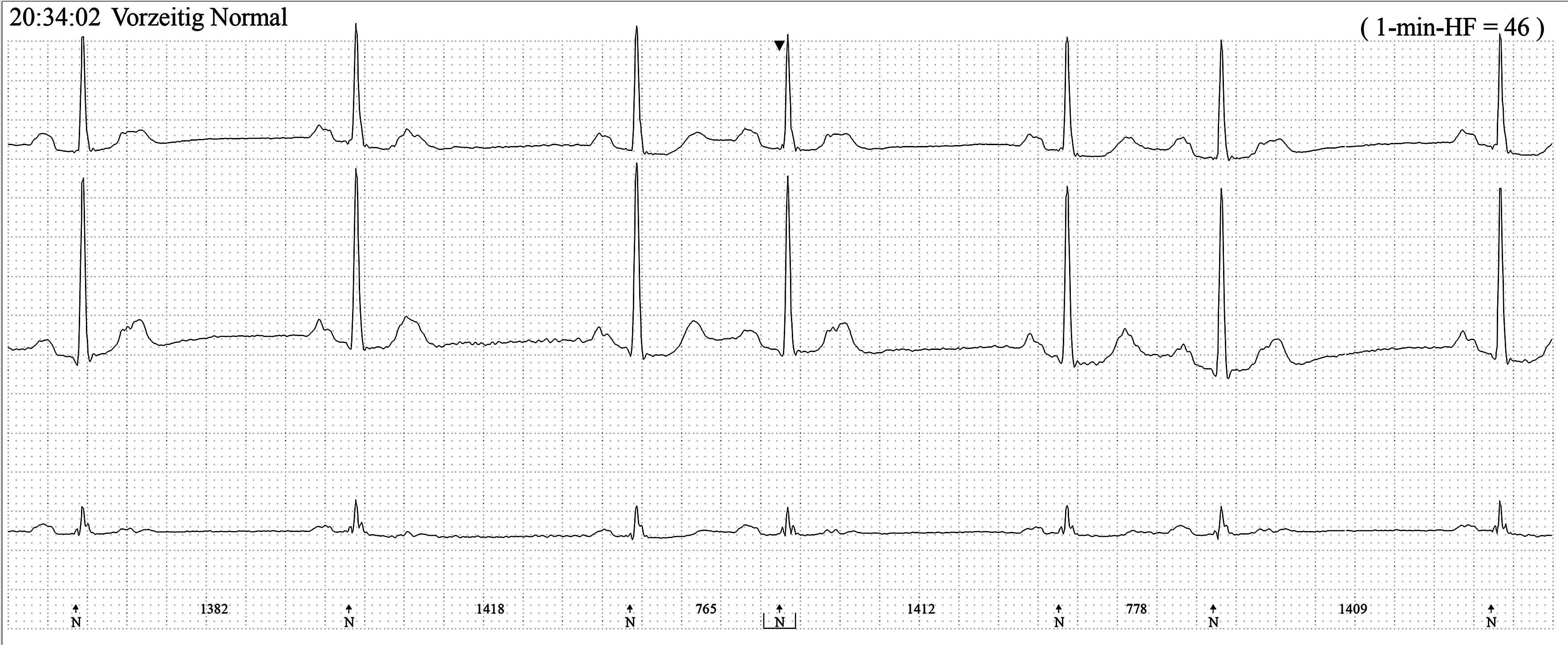
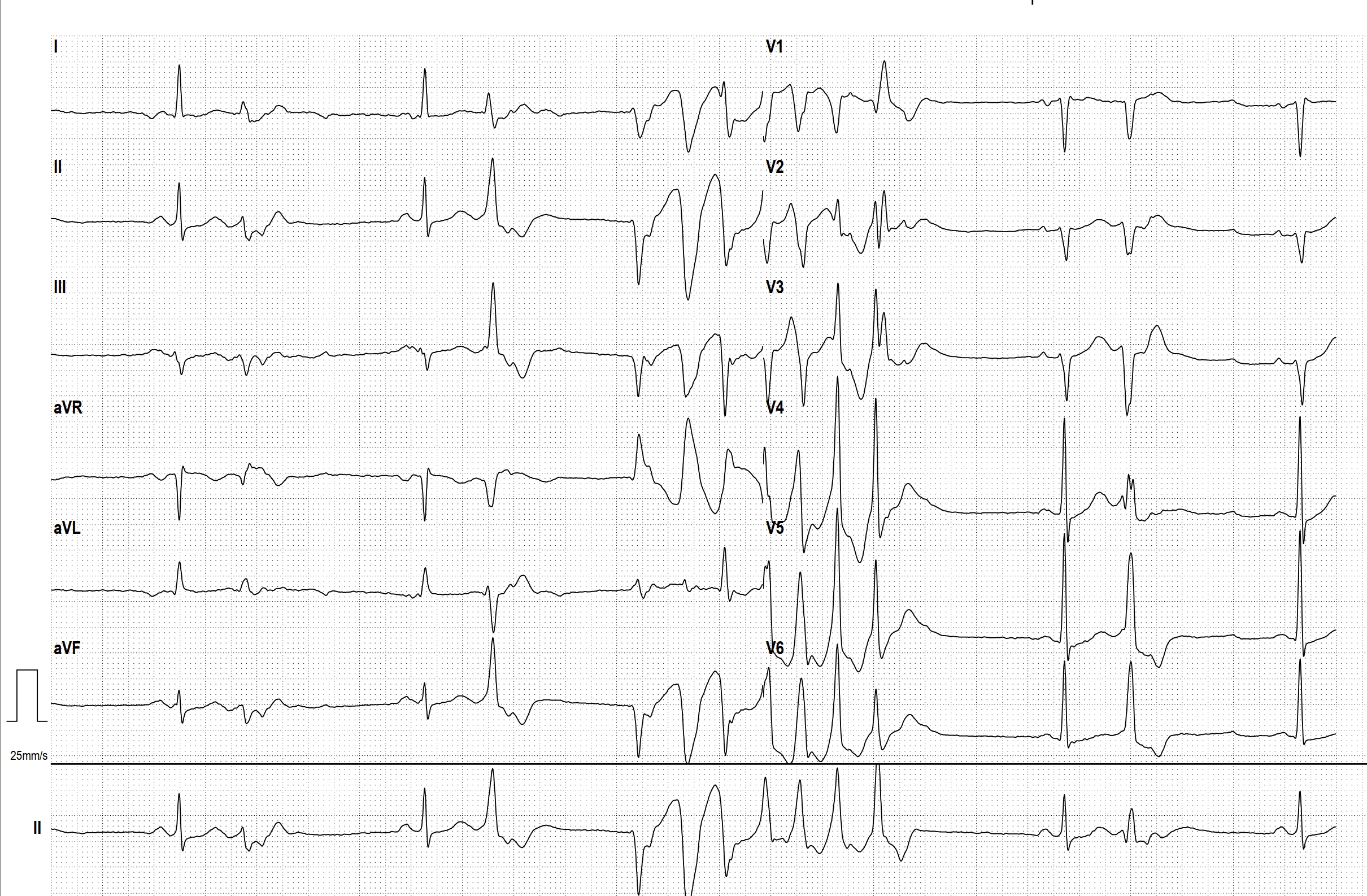
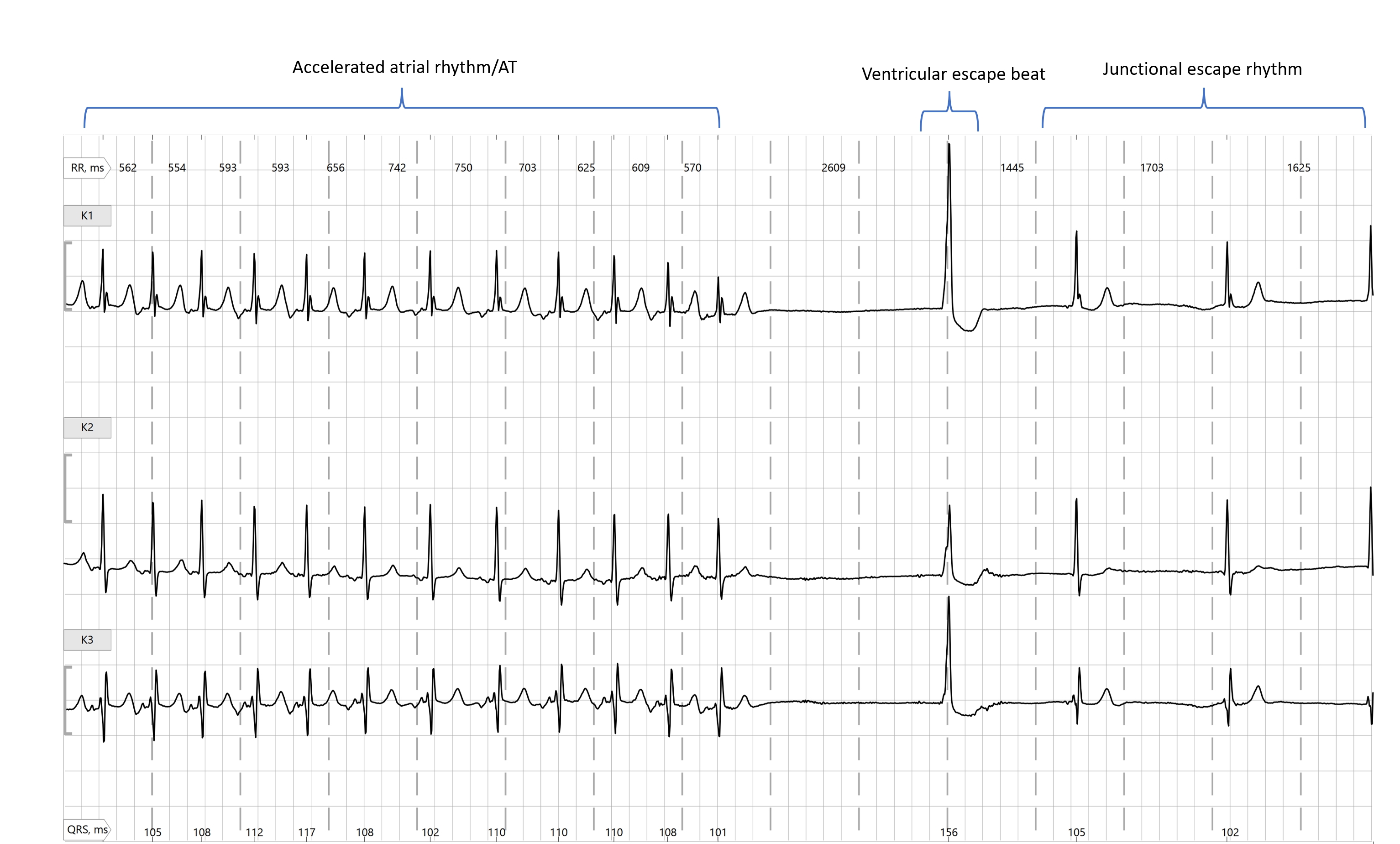
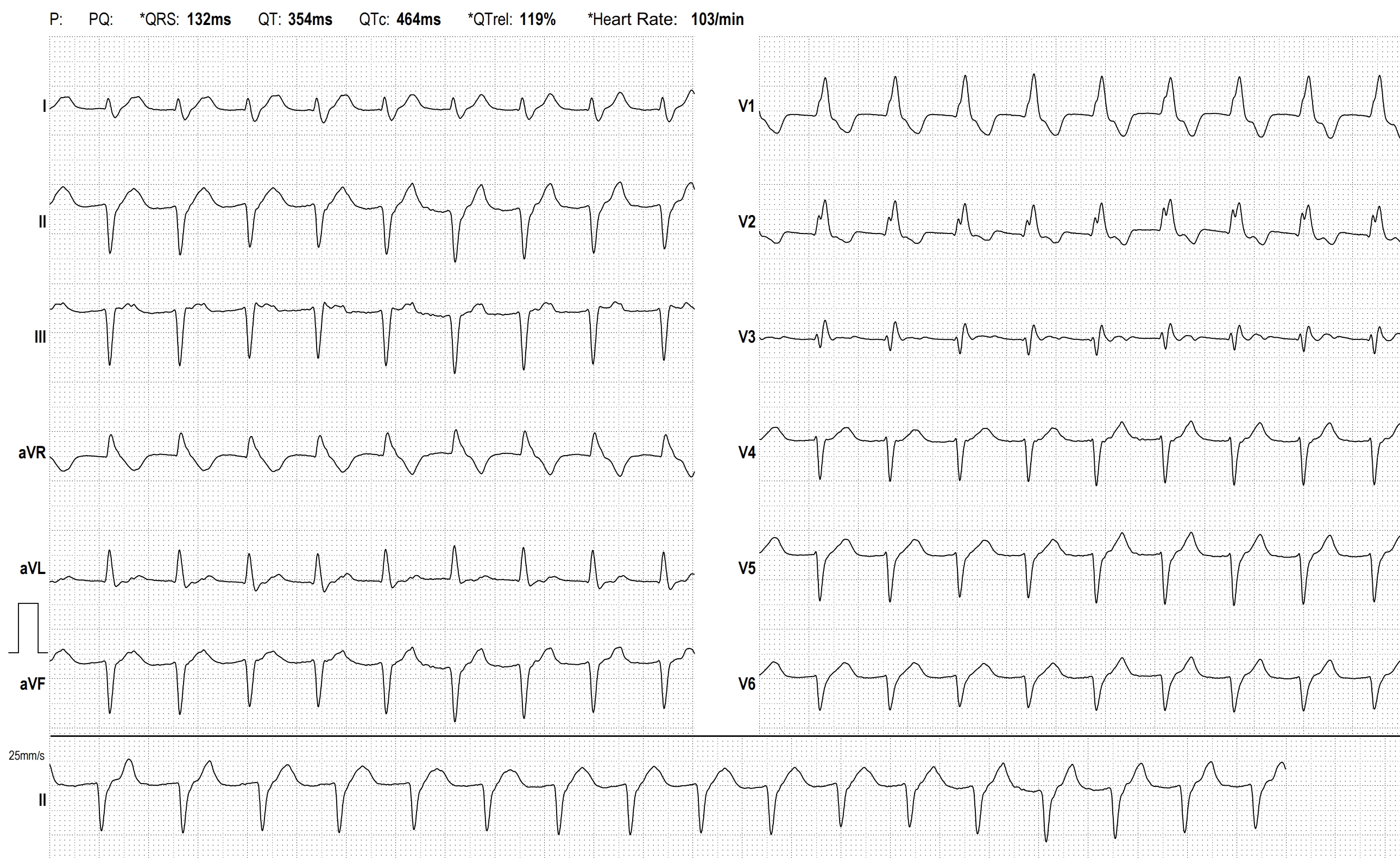
- SICK-SINUS-SYNDROME
- Smartwatch Rhythm Strip